Composition of gut microbiome drives granulopoiesis
Refer a colleague
Researchers demonstrate that changes in the intestinal microbiome stimulate neutrophil production in mice.
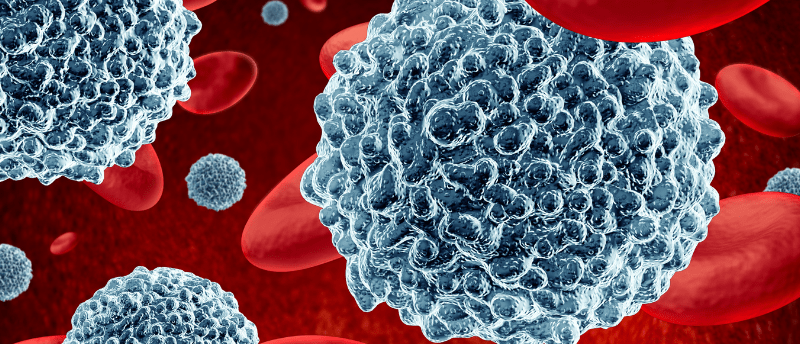
Neutrophils are the most common type of granulocyte, a type of white blood cell. A low neutrophil count is often seen in leukemia patients or following chemotherapy and is a condition called neutropenia. It is known that a process called granulopoiesis replenishes neutrophil count and researchers at Hokkaido University (Japan) have recently discovered that the gut microbiome is a key part of this mechanism. This provides a potential avenue for novel adjuvant therapies that help support a chemotherapy recipient’s immune system.
Instances of increasing granulopoiesis above a homeostatic level can be divided into two scenarios: emergency granulopoiesis, which is driven by the presence of bacteria, and reactive granulopoiesis, caused by the absence of an active microbial infection. Reactive granulopoiesis occurs after neutropenia caused by hematopoietic stem cell transplantation (SCT) or cancer chemotherapy.
To understand the mechanisms through which neutropenia triggers reactive granulopoiesis following SCT or chemotherapy, the researchers induced neutropenia in mouse models and monitored levels of cytokines that are known to be linked to granulopoiesis. They observed significantly raised levels of the granulocyte-colony stimulating factor (G-CSF) and interleukin 17A (IL-17A). Using IL-17A deficient mouse models, they then showed that the cytokine is crucial for replenishing neutrophil levels and confirmed that T cells are its primary source..
 Demystifying the immune system’s function as a spam filter
Demystifying the immune system’s function as a spam filter
We chatted with Javier Irazoqui about the brain-gut-microbiota axis, the challenges of studying these interactions and the techniques used to do so.
Prior research had suggested that the gut microbiome and bone marrow hematopoiesis could affect each other, so the researchers were interested in building on this and finding out if the gut microbiome influences granulopoiesis. By decontaminating the gut microbiome using antibiotics, they showed that T-cell production of IL-17A was suppressed and the typical increase in neutrophil numbers was not observed. Subsequent fecal transplantation from a distinct mouse experiencing neutropenia stimulated neutrophil recovery, showing that the gut microbiome upregulates reactive granulopoiesis via the IL-17A that is secreted by T cells.
Additionally, the researchers found that prolonged periods of neutropenia alter the gut microbiome. They concluded that this change in the microbiome composition stimulates reactive granulopoiesis.
Next, the team will look at clinical trials to see if this link between the gut microbiome and granulopoiesis occurs in humans. Patients receiving chemotherapy and experiencing neutropenia are often vulnerable to infection, so this research could lead to novel fecal microbiome transplant or probiotic therapies that support granulopoiesis. Furthermore, antibiotic formulations that do not impact granulopoiesis-supporting bacteria may also be devised to ensure neutrophil recovery is not affected.
Please enter your username and password below, if you are not yet a member of BioTechniques remember you can register for free.