See the light: treating bacterial infections with molecular machines
Visible light-powered molecular machines could be used to efficiently and effectively treat bacterial infections in vivo by physically disrupting the bacterial membrane.
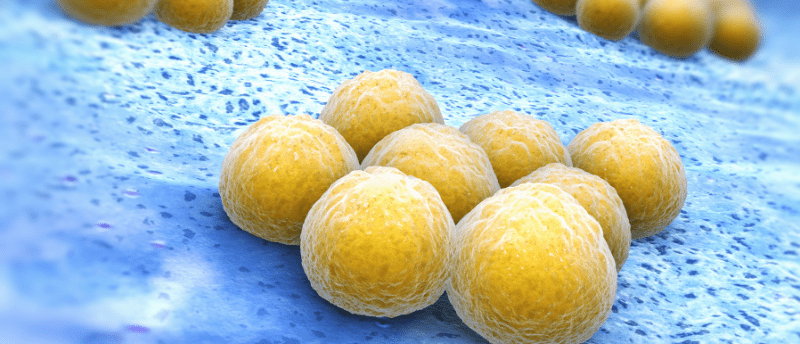
James Tour and fellow researchers from Rice University (TX, USA) have recently developed a molecular machine (MM) that utilizes visible light to puncture both gram-negative and gram-positive bacterial cell membranes. This MM uses visible light as its energy source, as opposed to UV light, which is harmful to humans upon prolonged exposure and could provide an alternative method with which to address the antibiotic resistance crises.
According to lead author Tour, antibiotic-resistant bacterial infections are a looming threat to human health: “I tell students that when they are my age, antibiotic-resistant bacteria are going to make COVID look like a walk in the park.” Even the successful treatment of infection overlooks aspects that can provide the basis of a new infection, such as persister cells, dormant bacteria that survive antibiotic treatment, and biofilms, clusters of bacteria. However, bacteria lack defenses against mechanical interventions, making MMs an attractive and efficient treatment for bacterial infections.
 No rejections for new islet transplantation method
No rejections for new islet transplantation method
Islet transplants for type 1 diabetes could soon have a lesser risk of rejection and remove the need for immunosuppression.
Researchers developed a MM that utilizes visible light at 405-nm as an energy source to break open bacterial membranes. Based on Bernard Feringa’s work (Stockholm University, Sweden), the current study’s MM spins the molecules’ rotors to act like a drill. Different amine groups are attached to enhance the associations between the MM and the bacterial membrane, allowing it to accurately target the cause of the infection and reducing collateral damage to healthy cells. Once the association is formed, the MM can puncture the membrane, killing the bacterium.
When applied to invertebrate models of burn wound infection, the visible light-triggered MM killed bacteria faster than conventional antibiotic treatments. What’s more, methicillin-resistant Staphylococcus aureus, a bacterium that can cause fatal infections of soft tissue, was killed using this new MM, a promising result when considering the use of MMs in public health treatments. Researchers also demonstrated that persister cells and biofilms could not evade the MM like they can when treated with conventional antibiotics. The research group is continuing to explore how to improve the targeting of the MM so that it only affects bacteria, avoiding damage to healthy human cells.
This new MM treatment could be used in conjunction with conventional antibiotics to allow for the effective use and resurgence of antibiotics that have been previously discontinued due to antibiotic-resistant bacteria. First author, Santos, reports, “Drilling through the microorganisms’ membranes allows otherwise ineffective drugs to enter cells and overcome the bug’s intrinsic or acquired resistance to antibiotics.”
The development of a visible light-triggered MM could provide a quick and thorough treatment for antibiotic-resistant bacterial infections without exposing humans to harmful UV light. Overall, this technique furthers our understanding of the roles MMs can play in supplementing known, and generating new, antibiotic treatments.