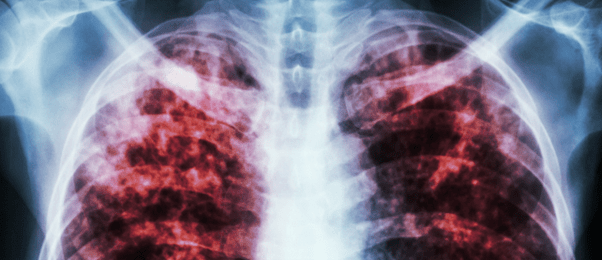
Old drug learns new tricks against small-cell lung cancer
Refer a colleague
In a mouse study telling a tale of old meets new, an experimental combination of two drugs has been found to stop the growth of small-cell lung cancer.
Small-cell lung cancer is one of the least treatable forms of cancer, and the only current treatment – platinum-based chemotherapy – adds a mere 2 to 6 months of life. A collaboration between researchers at Washington University School of Medicine (MO, USA), Grenoble Alpes University (France) and The University of Texas MD Anderson Cancer Center (TX, USA) has demonstrated a way to increase the effects of older chemotherapy drugs, potentially giving patients a better chance of survival.
Previously, a drug called cyclophosphamide was used to treat small-cell lung cancer, which works by causing a kind of DNA damage known as alkylation damage. Cyclophosphamide was replaced by platinum-based drugs in the 1980s, mainly due to their lesser side effects rather than significantly improved prognosis. Whilst both drugs initially stop cancer growth, they then start failing as the cancer develops resistance. Pinpointing just how resistance develops could lead to new treatment options.
The establishment of the current study was down to a pinch of luck. A few years ago, co-senior author Nicolas Reynoird (Grenoble Alpes University) and his team discovered that a protein called RNF113A may contribute to small-cell lung cancer; however, the function of this protein was unknown. At the same time, fellow senior author Nima Mosammaparast (Washington University School of Medicine) demonstrated that cancer cells utilize RNF113A to repair alkylation damage, the very damage that cyclophosphamide causes. The researchers teamed up to investigate how small-cell lung cancer cells resist alkylation damage and to see if they could boost the alkylating effects of cyclophosphamide.
 Meet the good virus: virotherapy for treatment-resistant cancers
Meet the good virus: virotherapy for treatment-resistant cancers
Researchers find that coupling virotherapy with two adoptive cell therapy techniques has the potential to fight treatment-resistant cancers.
The team discovered that RNF113A is regulated by a protein called SMYD3. The protein is highly expressed in small-cell lung cancers, and high levels of SMYD3 are associated with increased resistance to alkylating chemotherapy, more invasive disease and worse prognosis.
As healthy lung tissue had low levels of SMYD3, the team investigated whether they could target cancer cells by knocking down the protein. They created mouse models, by grafting cancerous cells from two patients with small-cell lung cancer onto separate groups of mice. One patient had not yet been treated, whereas the other patient had been treated with platinum-based therapy and their cells had developed drug resistance.
Following tumor growth, the mice were treated with either an inhibitor of SMYD3, cyclophosphamide, both or an inactive solution.
Cyclophosphamide alone initially stopped tumor growth, but the tumors grew back after a few months as the cells developed resistance. Inhibiting SMYD3 alone slowed down tumor growth to a certain extent. However, the combination of the SMYD3 inhibitor and cyclophosphamide stopped the growth of the tumors for the whole duration of the experiment.
Importantly, these results highlight a potential improved form of treatment for patients with small-cell lung cancer, who usually survive less than a year and a half after diagnosis.
“We’re talking to a number of other groups about starting a phase 1 clinical trial as soon as possible,” Mosammaparast concluded. “One of the challenges we will face is convincing doctors to go back to an old drug. But the nice thing about this strategy is that it may work where current therapies have failed. This treatment worked just as well against the tumor from the patient who had already relapsed on platinum-based therapy as it did against the untreated patient. People with small-cell lung cancer are in desperate need of better treatments, and I’m very excited about the possibilities here.”
Please enter your username and password below, if you are not yet a member of BioTechniques remember you can register for free.