Targeting the mitochondria as a new frontier in the fight against leukemia
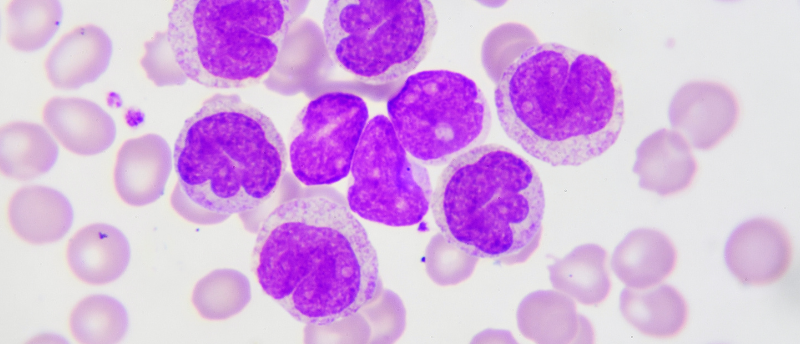
A novel drug candidate is yielding encouraging pre-clinical results as a potential chemotherapeutic by killing mitochondria in leukemia cells, whilst leaving healthy cells unaffected.
A collaborative effort of researchers from Rice University (Houston, TX, USA), led by Natasha Kirienko, and the University of Texas MD Anderson Cancer Center (Houston, TX, USA), led by Marina Konopleva, has resulted in the discovery of small-molecule candidates that are able to override the mitophagy bypass of cancer cells and trigger the breakdown of these renegade cancer cell mitochondria.
Mitochondria, present in every cell in numbers ranging from dozens to thousands, work tirelessly to regenerate ATP, an essential energy carrying molecule. Proper regulation of the mitochondria is vital to the maintenance of healthy cell processes, so it comes as no surprise that its dysregulation is linked to certain cancers.
Like a car engine or a power plant, mitochondria wear out over time and will eventually reach the end of their serviceable use. Mitophagy is the process of decommissioning and dismantling old mitochondria to make way for new and healthy replacements. However, in times of extreme need for energy, this process can be bypassed. Cancer cells, whose rapid and uncontrolled growth requires an endless source of energy, often exploit these intrinsic emergency mechanisms to maximize the amount of ATP available.
It has been found that leukemia cells follow this model and contain many more damaged mitochondria than equivalent healthy cells. Consequently, this means that leukemia cells are far more susceptible to further mitochondrial deterioration than healthy cells.
The research teams built on previous research in which they screened over 45,000 potential compounds for their potential as molecular inducers of mitophagy. By using a variety of in vitro experimental methods, they narrowed the field down to eight promising candidates.†
 Biochemists find a way to mend a broken heart
Biochemists find a way to mend a broken heart
Researchers developed a strategy to return cardiomyocytes to a stem cell-like state to promote the regeneration of heart muscle cells.
In this current study, the teams went further to probe the eight candidates with additional in vitro and in vivo experiments. A cytotoxicity assay conducted against acute myeloid leukemia (AML) cells identified that six of the eight compounds were able to trigger cell death. Following on from this, the six remaining candidates were tested against two other common types of leukemia cells. Five candidates survived this round of investigation, and each displayed far less harm to healthy cells.
In their final experiment, the team employed an emerging in vivo technique known as a patient-derived xenograph (PDX). In short, this involves taking AML cell samples from a patient and injecting the cells into the tissue of living mice. Once the mice displayed evidence of the disease, they were treated with one of or a combination of the candidates.
These mouse-model studies highlighted one candidate, PS127E as the most effective candidate at killing AML cells in a live model. PS127E is a benzylic compound containing substituent methoxy and nitro functional groups. Its bioactive function is to support the action of the kinase PINK-1, which is instrumental in triggering mitophagy, and mutated forms of the kinase have been indicated as potential sources for other diseases.
Whilst these results do sound promising the paper’s authors are the first to acknowledge that considerable research is still required before PS127E can be on the market as a chemotherapeutic. First, even though its target protein has been identified, more studies will have to be conducted to probe its full mechanism of action. Second, proper ADMET profiling will have to be conducted to determine safe dosage levels. Finally, whilst it has been shown to have a cytotoxic effect on specific types of AML cells, AML is a complex disease and multiple variations of AML cancers exist.
Further testing on a wide variety of AML cancers will be essential to discover which patients this novel therapeutic will be beneficial for. In her statement, Kirienko projects that they are still several years away from having sufficient evidence to take this candidate drug to clinical trials.