Improved preclinical drug studies with next-generation in vitro cancer models
Accurate cancer models are integral to the success of preclinical research yet have proven elusive. Mindy Goldsborough (ATCC, VA, USA) discusses the ongoing efforts to develop improved in vitro models.
The development of anti-cancer drugs, biologics and immunotherapies have been stymied by poor rates of success during the human clinical trial stage, in part due to the absence of a system of predictive, biologically relevant cancer models. Many traditional cancer cell lines have a high proliferative capacity and are easy to genetically manipulate, which has made these in vitro models an industry standard for testing hypotheses and performing high-throughput screening in preclinical studies. Yet, the results obtained from preclinical studies using these cell lines do not translate into useful treatments at a high enough rate. There are a number of factors that contribute to this.
Incumbent challenges
Firstly, many of the current in vitro models are monocultures; cell lines typically represent a single cell type from a single tissue, while tumors consist of a heterogeneous population of cells. Tumors also grow as complex 3D structures in the body that are difficult to replicate in vitro. In addition, many cell lines that are used in preclinical studies lack patient-derived clinical and genomic information. Further, the number of available continuous cell line models is insufficient to capture the genetic diversity of cancer. This makes it difficult to link the results of a study back to a particular patient population and results in poor predictive value to many patient populations. While use of continuous cell lines have an important place in basic research and preclinical testing, additional approaches are needed to augment the incumbent culture systems used to study cancer. Significant advances in the development of research models that are annotated with patient data are needed to meet key challenges faced by cancer researchers. Ideally, these models would solve the issues outlined above, permitting in vitro growth of cancer types previously not possible and providing essential tools for preclinical research. These models would also enable more positive therapeutic outcomes for patients by more accurately mirroring in vivo physiology.
These challenges were taken up by the Human Cancer Models Initiative (HCMI), a consortium of several major institutions that includes the two model development arms within the National Cancer Institute (NCI). The goal of the HCMI is to develop 1000 novel human cancer models that are paired with bioinformatics and patient clinical data, particularly from rare or underrepresented cancer types. Scientists within these institutions generated the protocols and studied the expansion capacity, cryopreservation ability, genetic stability, and feasibility of larger-scale bioproduction of the models generated. These next-generation models are now widely available for global distribution by ATCC, and more will be added over time.
Organoid and conditionally reprogrammed cell options
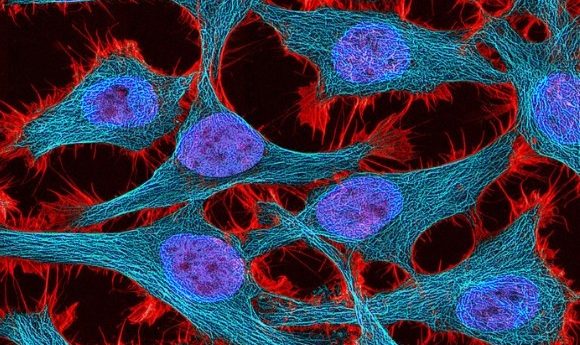
Offering scientists a wide variety of well-characterized, next-generation 2D and 3D patient-derived cancer models paired to critical patient data is key to identifying and targeting novel therapies and facilitating future translational cancer research. Two new technologies—organoids and conditionally reprogrammed cells (CRCs)—are purported to maintain an in vivo phenotype and the genetic heterogeneity seen in cancer. These features, coupled with greater molecular characterization and extensive clinical and genomic data, can significantly improve the foundations for pre-clinical research.
Organoids are culture models that are grown in an extracellular matrix and display 3D, organ-like ‘microtissue’ structures that may exhibit native cell types of the tissue of origin. ATCC will soon offer organoids derived from multiple types of human tissues such as colon, rectum, lung, stomach, pancreas, esophagus, and mammary that were developed by laboratories contributing to the HCMI. Organoid models typically can be maintained in culture continuously for at least 60 days and some models have been in culture for years.
In contrast to organoids, CRCs are 2D culture models. CRCs are created by culturing the cell of interest with a Rho-associated protein kinase inhibitor in the presence of irradiated mouse cells. This process is believed to transiently reprogram the cells to a de-differentiated phenotype and stimulates their rapid expansion. A major advantage of this system is that it eliminates the need for immortalization via transduction of viral or cellular genes. When moved into a culture that resembles their natural environment, CRCs then revert to a differentiated phenotype.
The next-generation models created at HCMI greatly improve on traditional continuous cell lines as cancer models. What these models provide is unique in that they allow scientists to study cancer under conditions that better resemble a tumor’s complex physiology. Further, the breadth and diversity of these advanced models coupled with the availability of the clinical patient and molecular characterization data through the NCI portal is set to advance cancer drug development, providing better predictability of clinical outcomes by better mirroring certain aspects of in vivo physiology. This, in turn will result in a more defined understanding of cancer biology and more targeted treatments for the diverse manifestations of the disease.