Blood type and cancer survival
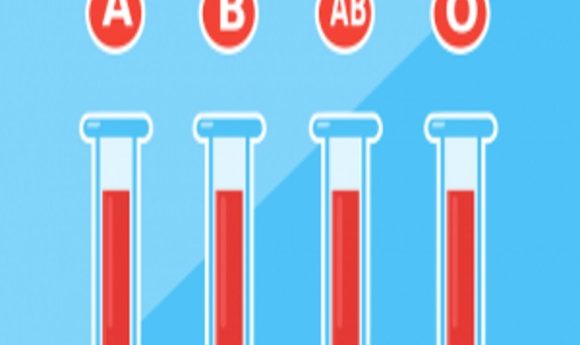
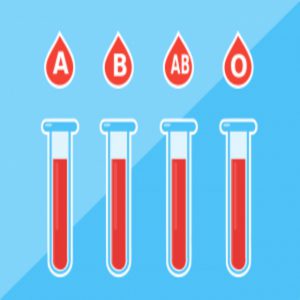
Previous studies have linked the blood type A with increased risk for ovarian cancer. A new study suggests it also may have something to say about one’s chance of survival after getting the disease.
According to the Centers for Disease Control and Prevention (CDC), each year approximately 20,000 American women are diagnosed with ovarian cancer. The disease is the fifth deadliest form of cancer—following lung, breast, colorectal, and pancreatic cancers—and Alicia Beeghly-Fadiel, an epidemiologist at Vanderbilt University, said there are few prognostic indicators for the disease.
“There have been a few genome-wide association studies (GWAS) that show that blood type is linked to your risk of getting a variety of different cancers, and one of them is ovarian cancer. Studies suggest that having blood type A makes you more susceptible to getting the disease,” she said. “I couldn’t help but wonder why blood type would have anything to do with cancer at all. And as I started thinking about what mechanisms might be behind it, I wondered if this marker might actually be more relevant to survival than risk.”
To test the idea, Beeghly-Fadiel and her colleagues collected data from the electronic medical records of more than 1000 confirmed cases of ovarian cancer and reviewed serologic assays of each patient’s blood to determine ABO variants. They then looked at links between overall survival and blood type, while controlling for potential confounding factors such as age, race, cancer stage, and grade. Given the previous work linking type A blood with higher cancer risk, the group hypothesized that they would see a worse survival rate. But they were surprised to see the exact opposite effect—type A blood was associated with a stronger chance of survival.
“I did a lot of extra checks to make sure that there were no confounds that might explain it,” she said. “But the genetics confirmed the finding. We had only exploratory analyses based on sample size, but they supported what we saw with the phenotype, which shows why also looking at genotype is so important.”
Beeghly-Fadiel is already planning to try to replicate this work with a larger cohort. Once she completes that, she plans to figure out the mechanism behind this link.
“Is it because these antigens that are expressed on the red blood cells aren’t just on the red blood cells that determine blood type but also on epithelial cells, like tumors? Maybe an apparent expression of the ABO antigens is somehow related to the progression of cancer? There are so many pathways that the ABO is involved with from coagulation to inflammation,” she said. “By figuring out the mechanism, we have the potential to figure out what may be targetable for treatment—or use it as a biomarker for prognosis.”