“Helper” T-cells pack more of a punch against tumors than first thought
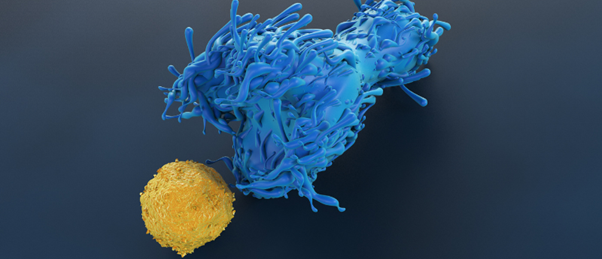
CD4+ T-cells, primarily considered to play a supportive role in the anti-tumor immune response, have been seen to actively kill cancer cells in a mouse model of melanoma.
A recent study by a team at the Peter Doherty Institute for Infection and Immunity (Melbourne, Australia), has revealed new insights into the role of CD4+ T-cells in anti-cancer immunity, using mouse models of melanoma and a series of imaging experiments. These findings reveal that CD4+ T-cells are more potent than previously thought in the tumor microenvironment, promoting the potential of their therapeutic use in the fight against cancers.
Melanoma is the 17th most common cancer globally, with 150,000 people newly diagnosed with the condition in 2020. So far, it has proved partially susceptible to the expanding range of immunotherapeutic treatments that have been emergent in the last few decades. However, cell-based immunotherapies such as CAR-T, which currently struggle in the treatment of solid tumors, have yet to be approved for the treatment of melanoma.
For decades, CD4+ T-cells were seen to have a primarily supportive role in the immune response to cancer, priming CD8+ T cells that would take the more active role in attacking cancer cells. However recent clinical studies have suggested that they may play a more important role in the immune response to cancer than initially thought.
Finding the perfect target: developing immunotherapies for melanoma
In this interview, we talk to Cristina Puig-Saus (University of California, Los Angeles, CA, USA) about her work developing T-cell therapies for melanoma.
To identify how active these cells are in the anti-tumor response, the team conducted a series of experiments in mouse models of melanoma, inoculating mice with melanoma cells engineered to express mCherry alongside a variety of different modifications. These models were then challenged with CD4+ T-cells engineered to express green fluorescent protein (GFP). Mice were anesthetized and subsequently operated on to expose the site inoculated with melanoma cells. Lastly, intravital two-photon microscopy was used to image the action of the CD4+ T-cells in real time, in vivo.
Using this approach in a series of different studies, the team identified that the CD4+ T-cells both infiltrated and attacked the cancer cells in the tumor microenvironment, suppressing and in some cases eradicating tumors, even when no other lymphocytes were present. Further in vitro and in vivo experiments revealed that the cells targeted cancer through several different pathways, including the tumor necrosis factor–α and Fas ligand pathways as well as by producing IFN-γ, which impacts cancer cells directly and stimulates the production of nitric oxide in myeloid cells, further damaging the tumor.
Commenting on the impact of these results senior author Thomas Gebhardt explained that, “while CD4+ T cells are often viewed as accessory cells regulating the function of other immune cells, our work shows they can work effectively on their own. Therefore, harnessing their potential therapeutically holds great promise for the development and improvement of current cancer immunotherapies.”