CTC-derived organoids establish new tool for investigation of metastasis
The successful cultivation of stable CTC-derived organoids has enabled an investigation into methods of survival and resistance in cancer cells.
A team of researchers from the German Cancer Research Centre, the Heidelberg Institute for Stem Cell Technology and Experimental Medicine and the National Center for Tumor Diseases Heidelberg (all Heidelberg, Germany), have successfully cultivated circulating tumor-cell (CTC)-derived organoids directly from blood samples of breast cancer patients. These CTC-derived organoids have allowed researchers to investigate the molecular signaling pathways that ensure cancer cells’ survival and resistance to treatment. Through this, the team discovered the protein NRG1 as a key signaling component for CTC survival.
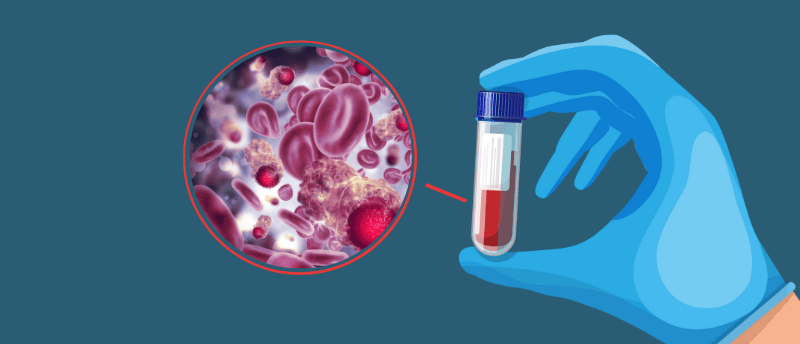
The treatment and prognosis of breast cancer have greatly improved in recent years; however, metastatic breast cancer remains incurable. The lungs, liver, lymph nodes and brain are some of the most common locations to which breast cancer spreads, with CTCs highlighted as a likely candidate for the cause of these metastases. CTCs are cancer cells that detach from the primary tumor and spread to other body parts through the bloodstream, making them difficult to isolate and investigate. With CTC lifespan suggested as a key parameter controlling metastases, identifying pathways responsible for CTC survival and resistance is crucial to developing our understanding of metastasis.
What’s more, to fully understand how tumor cells survive and acquire adaptive resistance mechanisms, researchers need to be able to collect tumor material over the course of the disease. Taking regular tumor biopsies may prove complex and even prohibitive, making CTCs that can be obtained from simpler blood samples an even more attractive option for researchers. However, isolating CTCs and multiplying them in the laboratory has proven time-consuming and laborious, requiring the complex and lengthy process of propagating the CTCs from patients in immunodeficient mice. Therefore, the establishment of techniques to support the stable and reliable isolation and expansion of CTCs would be hugely beneficial for the investigation of metastasis and tumor cell development.
The team set out to establish a method for the long-term expansion of CTCs from liquid biopsies of breast cancer patients. They started with a test of the efficacy of a G1 medium in supporting CTC expansion directly from liquid biopsies of breast cancer patients. However, this was deemed insufficient to promote cell proliferation and survival of CTCs in vitro. To find the optimal conditions, transcriptomic analysis was performed with the aim of identifying molecular pathways critical for CTC growth in vivo.
The team found NRG1 to be strongly enriched in lung-colonizing cells when compared to the primary tumor. Subsequent supplementation of G1 with NRG1, along with other factors, allowed for the exponential growth of CTC-derived organoids over time.
Further analysis into NRG1 revealed that it binds directly to the HER3 receptor on cancer cells and, together with the HER2 receptor, activates signaling pathways that ensure CTC growth and survival. When these receptors are blocked, compensatory signaling from FGFR1 is activated to ensure CTC growth and survival.
“With the help of such ‘bypasses’, tumors react to external influences, for example to targeted therapies against HER2. This is a crucial mechanism in the development of therapy resistance,” explained lead author Roberto Würth.
When the team looked into combined inhibition of NRG1 and FGFR1 signaling they achieved the elimination of CTC-derived organoids in vitro and impaired tumor formation of mice in vivo.
Further testing into this method is required, however, it shows promising results for developing easier methods to investigate cancer cell survival and provides opportunities to create customized therapies.