Cytokine-based cancer immunotherapy: current progress and future prospects
Cancer immunotherapy is an evolving field of research. Cytokines are a key area of interest in cancer immunotherapy; however, challenges are faced when translating their use from the lab to the clinic. In this interview, Shuang Zhou discusses the current landscape of cytokine-based cancer immunotherapy and looks ahead to the future of the field.
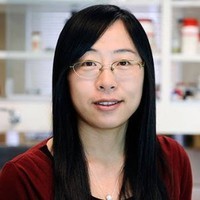
Shuang Zhou is a Product Manager at the US subsidiary of the global biotechnology company Sino Biological, Inc. (Beijing, China), a manufacturer of high-quality research reagents, where she manages the drug target product portfolio. Before joining Sino Biological, Shuang was a Senior Scientist in the biopharmaceutical industry. She completed postdoctoral studies at Harvard Medical School (MA, USA), Beth Israel Deaconess Medical Center (MA, USA), and Baylor Scott & White Health (TX, USA) in cancer biology and pharmacology after obtaining her PhD degree in Pharmaceutical Sciences from North Dakota State University (USA).
Could you summarize the role cytokines play in cancer?
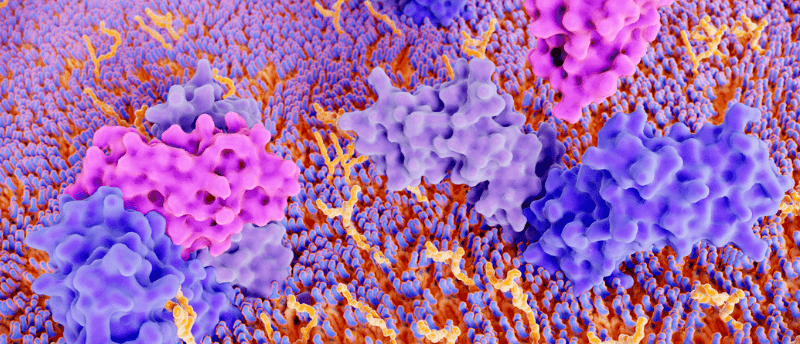
Cytokines are molecular messengers released by cells to regulate cell interactions and communications. As potent and complex immune mediators, they may either promote tumor growth and spread or mediate the antitumor immune responses.
Elevated levels of various cytokines, such as IL-1, IL-6, TNF-α, FGF and G-CSF, have been found in biosamples of cancer patients. During cancer formation, cancer cells release various cytokines and growth factors and recruit and reprogram other types of cells into their surroundings to establish a tumor microenvironment (TME) conducive to cancer growth. These cytokines may also induce normal cells, such as tumor-associated macrophages and endothelial cells, to produce additional cytokines that support the pathological process.
On the other hand, as part of the immune response, cytokines released in response to infection, inflammation and immunity can inhibit cancer development and progression. Because of the critical roles of cytokines in cancer, there has been considerable interest in harnessing cytokines for the diagnosis and treatment of cancer over the past decades.
What are some of the techniques that are used to investigate the role of cytokines in cancer?
The detection and quantification of cytokines can be achieved by a series of techniques, including functional bioassays, protein microarrays, high-performance liquid chromatography (HPLC), sandwich enzyme-linked immunosorbent assay (ELISA), enzyme-linked immune absorbent spot (ELISpot) and FluoroSpot assays, Meso Scale Discovery (MSD) electrochemiluminescence and bead-based multiplex immunoassays (MIA).
The analyses of cytokines are usually performed using serum, plasma, cell culture supernatants and tissue lysates. The selection of techniques to detect and analyze cytokines should be based on the type of samples, the number of analytes, the reliability of the methods and the sensitivity and specificity required. ELISA remains a popular technique for cytokine detection because it is quantitative, easy to perform and relatively inexpensive. ELISA kits and antibody pairs for cytokine sandwich immunoassays and multiplex systems are widely available to be used.
What’s the current landscape of cytokine-based cancer immunotherapy?
Cytokines as monotherapy have not fulfilled the initial excitement they induced. IFN-α was the first human immunotherapeutic approved by the US FDA for cancer as early as 1986. High-dose IL-2 (HDIL-2) was approved for the treatment of metastatic renal cell carcinoma (1992) and later for metastatic melanoma (1998) by the US FDA. However, both agents are currently less commonly used because of severe dose-limiting toxicities.
At present, the biological roles of many inflammatory cytokines have been deeply explored. Some of these cytokines, such as GM-CSF, IFN gamma (IFNγ), IL-7, IL-12, IL-15, and IL-21, have been considered ideal targets for antitumor therapies and are being evaluated clinically. To circumvent the side effects and improve efficacy, cytokines are being investigated clinically with new approaches, such as structural modification, localized delivery and combinational therapy with other regimens.
How can cytokines be utilized in cancer immunotherapy?
Cytokine therapy to activate the immune system of cancer patients has been an important treatment modality and continues to be a pivotal contributor to current cancer immunotherapy. As cytokines in the TME shape host immunity, therapeutic manipulation of the cytokine environment is a strategy to potentiate protective immune responses. Systematic or local administration of specific cytokines, e.g., IFN-α and IL-2, has shown clinical benefits. Novel cytokine mutants (superkines) and chimeric antibody-cytokine fusion proteins (immunokines) have shown superior efficacy and safety profiles compared to the original cytokines.
In contrast, specific cytokines released to the TME may promote all phases of tumorigenesis. In this regard, strategies to neutralize the pathogenic activity of such cytokines, e.g., M-CSF, can be developed to enhance cancer immunotherapy. The detrimental activities of immunosuppressive cytokines can be blocked by small molecules, antagonistic antibodies, cytokine traps or siRNAs.
In addition to single-agent therapy, cytokines may also be used in conjunction with other immunomodulatory drugs, such as adoptive cell therapy, cancer vaccines, checkpoint inhibitors (anti-CTLA-4 or anti-PD-1/PD-L1) and cancer-directed monoclonal antibodies.
How can cytokines be used in adoptive cell therapy?
Adoptive cell therapy (ACT), also known as cellular immunotherapy, is a form of treatment that uses the cells of our immune system to treat cancer. ACT includes different cellular approaches, including tumor-infiltrating lymphocyte (TIL) therapy, engineered T cell receptor (TCR) therapy, chimeric antigen receptor (CAR) T cell therapy, and natural killer (NK) cell therapy. Currently, ACT therapies targeting CD19 and BCMA have been approved by the US FDA. It is well recognized that cytokines and their receptors play pivotal roles in regulating ACT cells’ functional and phenotypic features, such as persistence, trafficking, memory cell formation, survival and proliferation. Cytokines, e.g., IL-2 and IL-2 superkine, have been used to enhance the in vivo survival and expansion of adoptively transferred anticancer TIL and CAR cells.
Genetical manipulations of different cytokines and their receptors in ACT cells have also shown promise in boosting ACT cells’ efficacy against various types of cancers. For example, a truncated cytokine receptor that lacks a specific intracellular domain can be incorporated into CAR-T cells. These receptors can block signal transduction of inhibitory cytokines and thus enhance the persistence and effector function of CAR-T cells.
How can cytokines be used in the development of cancer vaccines?
Cancer cells can be genetically modified to express specific cytokines to stimulate the host immune response, thereby acquiring the capacity to function as cancer vaccines. Provenge®, a US FDA-approved cancer vaccine, is developed from autologous dendritic cells loaded with an engineered fusion protein of prostatic acid phosphatase and GM-CSF. The GM-CSF-secreting whole tumor cell vaccine has been reported to induce strong T cell responses and inhibit tumor growth by recruiting and activating antigen-presenting cells at the injection site.
The use of cytokines in cancer vaccine formulations is becoming more prevalent. GM-CSF, IFN-α, IFN-γ, IL-2, IL-12, IL-15, IL-18 and IL-21 have shown immunological efficacy when used as part of a vaccine adjuvant strategy.
Apart from being the therapeutic targets, how are cytokines applied in cancer research?
As essential messengers that affect nearly every biological process, cytokines are also involved in cancer diagnosis and prognosis, stem cell differentiation, vaccine efficacy and allograft rejection. In addition, cytokines are involved in establishing 3D culture organotypic models from stem cells. In the presence of specific cytokines and growth factors, organoids can be grown from patient-derived healthy and tumor tissues, which are revolutionizing patient-specific drug testing and personalized medicine.
What challenges remain for cytokine-based cancer immunotherapy, and what are your hopes for the future of the field?
It is clear that therapeutic targeting of cytokine pathways holds great promise for cancer treatment. However, there are several factors that have limited the use of cytokines in cancer therapy, including: 1) lack of danger signals for systemic cytokine blocking; 2) severe side effects due to the pleiotropic nature and functional necessity of cytokines for multiple cell types; 3) the production and manufacturing of biologics is relatively expensive; 4) in contrast to chemical drugs, recombinant cytokines usually have limited shelf half-life and require special handling conditions.
Therefore, the search for next-generation cytokine-based drugs is mainly in three directions. Firstly, fine-tuning of the pharmacological properties is required for successfully developing cytokines into effective and safe cancer immunotherapy. For example, structure-modified superkines with increased binding affinity for select receptors are being evaluated for the effects in increasing antitumor responses and decreasing immunosuppressive cells.
The second concept would be to confine the effects of the cytokines to the site of action to avoid systemic pro-inflammatory effects. Strategies such as local or cavitary cytokine administration, chimeric antibody-cytokine fusion proteins or infusion of anti-cytokines in association with cytokines are being investigated to reduce the potential side effects.
Additionally, developing synergistic combinations, such as with the approved anti-PD-1/PD-L1 monoclonal antibodies and CAR-T cells, is a hot research area. The excitement in this field has resulted in a number of ongoing clinical trials. Studies have shown that cytokines may synergize with other cancer therapies, including anticancer vaccines, checkpoint inhibitors and cancer-directed monoclonal antibodies, to become formidable partners in cancer treatment. The feasibility of this approach awaits the future to reveal.
Sino Biological has developed a comprehensive bank of cytokines and receptors reagents, including recombinant proteins, antibodies, ELISA kits, antibody pairs and gene products, to support the research in this promising field.
In association with Sino Biological.