Giving T cells more charge: mitochondria fuel fight against cancer cells
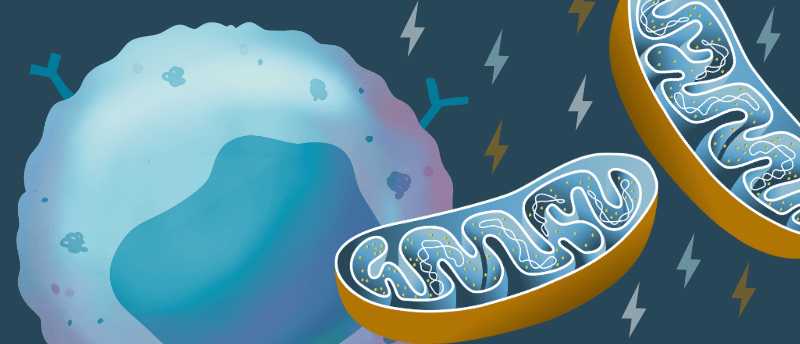
Scientists are supercharging T cells with multipotent stromal cells’ mitochondria to make them more ferocious invaders of the tumor microenvironment.
An international collaboration between researchers at Brigham and Women’s Hospital (MA, USA) and Leibniz Institute for Immunotherapy (Germany) has developed a method to give T cells more energy to penetrate the tumor microenvironment. By giving T cells more energy, the team is hopeful that they might be less susceptible to exhaustion, improving current immunotherapies.
T-cell exhaustion is driven by mitochondrial loss and dysfunction, posing a significant barrier to T-cell-based immunotherapies. T-cell therapies have been very effective against malignancies in the blood; however, they have proven less effective against solid tumors. This is in part because the tumor microenvironment can cause disruption to normal mitochondrial activity, causing T-cell exhaustion.
Previous research has suggested that intercellular mitochondria transfer is a viable option for overcoming this issue, but the process by which this is achieved has been less clear as many methods for mitochondrial transfer result in these mitochondria being hijacked for the cancer cells’ use.
“Previous efforts to enhance mitochondrial function in T cells have focused on targeting specific genes or pathways, but these methods fall short when the mitochondria are already damaged or dysfunctional. Our approach involves the transfer of whole, healthy mitochondria organelles into the cells. This process is comparable to organ transplantation—like heart, liver, or kidney transplants—but conducted at a microscopic level,” explained Luca Gattinoni (Leibniz Institute for Immunotherapy), co-leading author of the study.
Metastasis-associated macrophages identified
Several subsets of macrophage have been found to closely associate with metastasis-initiating cells in the tumor microenvironment.
One way for mitochondrial transfer to occur is via tunneling nanotubes, which are membrane protrusions that can bridge cells over vast distances and pass cytoplasmic components back and forth. Using an array of electron and fluorescent microscopy techniques, the current research team observed that exogenous mitochondria from bone marrow stromal cells can be passed to cytotoxic T cells via these tunneling nanotubes. They found that optimal mitochondrial transfer to the T cells occurred when Talin 2 – a cytoskeleton protein involved in actin filament assembly – was expressed by both the donor and recipient cell.
Following mitochondrial transfer to the T cells (mito+), the researchers infused the mito+ cells into a mouse model of melanoma. Here, the T cells with extra mitochondria demonstrated higher antitumor responses and prolonged survival compared to T cells without extra mitochondria. The researchers conducted numerous other experiments, which revealed that mito+ cells could penetrate solid tumors and persist without becoming exhausted in the tumor microenvironment. Applying this supercharging method to human lymphocytes and CAR-T cells displayed augmented cancer-destroying properties in cancer models.
The authors suggest that future applications could include using patient-matched bone marrow stromal cells to supercharge T cells for adoptive cell therapies. Additionally, this study builds a foundation for organelle medicine, inspiring the development of next-generation cell therapies.