Mapping and preventing tobacco use

 Kimlin Ashing tells us about the socioeconomic context of tobacco retailers, the targeting and use of e-cigarettes and the potential health impacts on future generations.
Kimlin Ashing tells us about the socioeconomic context of tobacco retailers, the targeting and use of e-cigarettes and the potential health impacts on future generations.
Ashing, PhD, a population and behavioral scientist at City of Hope (CA, USA), presented her research at the AACR Virtual Annual Meeting (27–28 April 2020).
Please tell us about yourself and the research you presented at the AACR Virtual Annual Meeting?
My life’s work over the past 30 years or so has focused on addressing cancer risk towards improving health and patient outcome, and I have a strong passion for eradicating health disparity. Tobacco is a known carcinogen. We’ve known this for over five decades. It’s a toxic substance that causes many types of cancers, including lung, of course, head and neck and other cancers as well as other chronic diseases, including chronic obstructive pulmonary disease. So, we wanted to understand the availability of these toxic products in communities and neighborhoods that surround our cancer center.
Why did you decide to conduct this study and how did you design it?
Given the known carcinogenic property of tobacco and that it is sold in retail, we wanted to understand the availability of products according to various community characteristics including race/ethnicity and income. We went about designing the study to have a broad impact. We are building a program of tobacco control research that hopefully has relevance to science, clinical practice and care, patients, as well as community because if we are trying to implement, for example, a tobacco cessation program for cancer patients, we have to understand what are their cues to smoking and that could be personal, social cues. Or, it could be community cues.
We used a geospatial analysis approach because we wanted to record the proximity of where they are located as well as the density of these tobacco shops. So, we had a very multidisciplinary team. We call it a team-science approach. We had epidemiologists, pulmonologists, tobacco cessation specialists and public health specialists on the team as well as cancer biologists because we wanted to have broader translational impact. We want to find out how different ethnic groups are impacted by genetic mutation around vulnerability to tobacco as well as how we metabolize tobacco and what some of the genotoxic effects are that later on lead to cancer and other diseases.
Can you tell us about the community surrounding your cancer center?
It’s in Southern California (USA) in a city called Duarte. It’s housed within a public health service planning area that is highly minority dense. About 40% of people are Latino Hispanic, about 23% Asian, about 6–7% African-American and there is a very wide range of socioeconomic status (SES), from a very wealthy enclave within our catchment area as well as very low income, lower SES communities, and those are the communities that we found were most burdened by the density of dedicated tobacco retail establishments.
We excluded groceries that, in the US, do sell tobacco products because we wanted to focus on those that market only these tobacco-related products. We found that there were almost 200 dedicated tobacco shops in our immediate catchment area.
We found that in some communities – especially with lower SES or social status and communities that were more minority dense, especially Latinos and African-Americans as well as Asians – there were up to two dedicated tobacco retail shops per square mile; that’s almost every two stoplights, you have a tobacco retail. If someone is trying to quit, and there are bombardments of cues to a substance that you’re using, it makes it very difficult for these persons, including cancer patients, to quit. And it makes it very difficult for that community to resist tobacco and implement tobacco control.
 Tobacco and vaping: predicting and preventing use across the USA
Tobacco and vaping: predicting and preventing use across the USA
<< Read more about Ashing’s study here >>
If you were to repeat this study in different states across the USA, do you think you would see a similar result?
Unfortunately, yes, we expect to get similar results. Others have done large studies, looking at geospatial analysis. Some studies have been done on the East Coast in Pennsylvania and other states – especially regions that have high tobacco production and consumption, so similar patterns are shown for low SES communities, where there is a greater density of dedicated tobacco smoke shops compared to wealthier neighborhoods. In fact, we found that very wealthy neighborhoods with annual household incomes of greater than US$90,000 actually had no dedicated tobacco shops within their communities.
What were the key conclusions that you drew; did they shock you or were they what you were expecting to see?
It was shocking, actually. I did not expect to see zero tobacco shops in those very high-income communities, and that means that they are well protected. Their schools are protected, the community centers are protected, their parks are protected. Their lives are better protected from tobacco exposure.
Whereas, lower income communities and these communities that already have health vulnerabilities and lack of resources have more dedicated tobacco shops. Additionally, they actually sell these products at a slightly cheaper price than in other neighborhoods.
So something has to be done. There are clear opportunities here for regulations and policy around where tobacco shops can be located to protect communities, especially economically and medically vulnerable communities and how these are marketed, for example, lower price for those communities.
What do you hope that these results will now inform?
We are hoping to have broad impact; we presented at the AACR Virtual Meeting and I was honored to be invited on a plenary session. We definitely informed science; we hope that it informs clinical practice, so that clinicians, physicians and nurses are aware of these disparities and where tobacco is located and available for communities, especially their patient population.
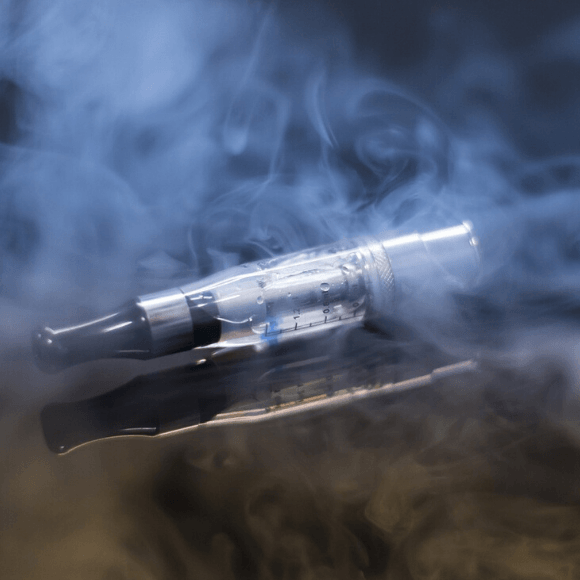
Tobacco products, especially the electronic delivery device and nicotine delivery device, are targeting youths and creating a new set of nicotine users, as the use of traditional cigarettes declines.
Therefore, we also hope that it alerts parents and teens that they are being specifically targeted, as well as teachers and community activists, so that they can be informed and have the data to work with their city council, local policymakers and state and national policymakers to protect their communities. We definitely want tobacco-free kids.
 Are cancer patients more vulnerable to severe outcomes of COVID-19?
Are cancer patients more vulnerable to severe outcomes of COVID-19?
A front-line view of cancer treatment in the global COVID-19 outbreak provides an insight to the rate of infection and lethality of SARS-CoV-2 infection in cancer patients.
What do you think is necessary to bring about the change and less consumption of these products?
Something that has worked but is a challenge in terms of regulation is increased taxes and costs on products. Higher prices usually mean that there is less of a desire in terms of purchasing because the cost can be prohibitive and that does protect some communities. I think that’s particularly important based on what I mentioned in terms of the lower price in economically challenged communities.
Also, what we and others have found is that US Hispanic and Latino youths are using prepackaged, disposable e-cigarettes. They are less costly. White youths are using e-cigarettes more than any other youth group, but they are also using more expensive devices, whereas the cheaper disposable devices are being used by minority youth and poor communities.
We need to understand what population is most vulnerable to what types of products so that policies and regulations could be targeted and tailored to those communities and the product that’s being marketed.
We need policymakers and legislators to be on board with this. We certainly plan to share this information with the state cancer control plan so that they could be more informed and then hopefully be able to use more sophisticated statistical analysis to look at if the density of these tobacco shops is also related to lung cancer incidents and even mortality.
Could you summarize the next steps for you and for your research?
We will use additional analyses to look at lung cancer rates and mortality, especially among adults because it would take some time to look at that trend in the youth population. It could take several years of development in terms of cancer, but we could also look at some of the other chronic diseases that develop sooner, such as heart disease and other types of lung disease.
We also hope to use this data to integrate in a broader tobacco cessation, tobacco control set of research. Our undertaking is looking at the genotoxic effects. We also want to work with clinicians and physicians to develop interventions that are considerate of tobacco exposure in communities because it will help improve the patient centeredness and empathy around the bombardment that some patients have in terms of trying to quit.
Is there anything else you want to add?
It’s shocking how many high school students have ever used an e-cigarette. Based on what others have found and the national data, we discovered that over 3 million high school students said they have used or tried e-cigarettes and half-a-million middle school students have too – kids who are nine and ten years.
This product has hit the youth population really, really hard. I believe that science will eventually show that these electronic nicotine delivery devices deliver carcinogens, toxins – there will be a new set of lung cancer rates. Currently, lung cancer has been on the decline as traditional smoking has been on the decline, and early detection and screening for lung cancer is increasing. These new electronic delivery systems are already creating lung diseases that challenge the health system. We must be prepared to limit availability to reduce use as well as treat these patients.