Let there be light: gene therapy targets cancer cells’ mitochondria
A light-induced gene therapy can damage cancer cells’ mitochondria, triggering widespread cancer cell death.
Researchers at Ohio State University (OH, USA) have developed a light-induced gene therapy called mLumiOpto, which targets cancer cells and activates electrical currents to damage their mitochondria. In mouse models, they have shown that this technology can shrink brain and breast tumors, offering a promising therapeutic modality to pursue further.
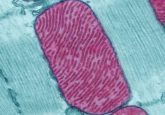
Mitochondria are known as the powerhouses of the cell; it’s no surprise, then, that successfully targeting them causes extensive damage to the cell. However, until recently, mitochondria were notoriously difficult to target due to their impermeable inner membrane. Previous research by co-lead author of the current study Lufang Zhou revealed that the mitochondrial inner membrane has a vulnerability – the electrical charge differential responsible for maintaining the membrane’s structure and function.
They previously demonstrated that they can disrupt this membrane charge by introducing a light-activated protein that creates electrical currents, activating it with an external laser. Now, the team has taken this work to the next level, developing a method for activating this electrical disrupter protein internally. They built an adeno-associated virus particle carrying genetic information encoding the positive charge disrupter protein – CoChR – and a bioluminescence-emitting enzyme.
These viral particles are delivered to cancer cells, where the genetic contents are expressed in the mitochondria. A follow-up injection is administered containing a chemical that induces bioluminescence of the previously delivered enzyme, which provides a light source that activates CoChR and leads to mitochondrial membrane damage and eventual cancer cell death.
Microbial trojan horses: disrupting the tumor microenvironment
Pedro Correa de Sampaio discusses the potential of Neobe’s synthetic biology platform in developing effective tools for making solid tumors more easily susceptible to cancer therapeutics.
The next piece of the puzzle was working out how to target these viral particles to cancer cells specifically. To achieve this, the researchers implemented multiple different systems. They added a promoter protein to the viral particle that enhances its expression in cancer cells only. They built their viral particles using human cells, which encapsulate the gene-packed virus within a natural nanocarrier that ensures stability in the human body. Finally, they also developed a monoclonal antibody – which they attached to the nanocarrier – that specifically binds with cancer cell-surface receptors.
“This monoclonal antibody can identify a specific receptor, so it finds cancer cells and delivers our therapeutic genes. We used multiple tools to confirm this effect,” explained X. Margaret Liu, co-lead of the study. “After constructing [adeno-associated viruses] with a cancer-specific promoter and a cancer-targeting nanoparticle, we found this therapy is very powerful to treat multiple cancers.”
They tested mLumiOpto in mouse models of brain and breast cancer, finding that the light-induced gene therapy was able to significantly reduce the tumor burden in treated mice compared to untreated mice. In the brain cancer mouse model, they also found that the treatment extended mouse survival. Further imaging studies confirmed that the gene therapy was targeted to cancerous tissue. The monoclonal antibody attached to the nanocarrier not only served to direct the nanocarrier to cancer cells, but also ignited an immune response against cancer cells.
The team is continuing their research, further investigating mLumiOpto’s potential in glioblastoma, breast cancer as well as other cancers.