Mobilizing CD4+ T cells and microglia against glioblastoma
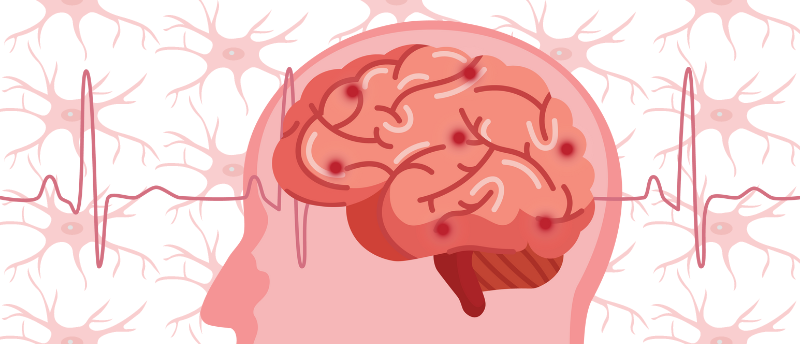
Researchers discovered that an immunotherapy, called anti-CTLA-4, mobilizes microglia against glioblastoma as it causes CD4+ T cell infiltration of the brain.
A study led by Salk Institute (CA, USA) scientists has shown that a type of immunotherapy, called anti-CTLA-4, increases the survival of mice with glioblastoma. For a cancer that currently has no effective treatment options, this finding has sparked hope.
Glioblastoma is the most common and aggressive form of brain cancer, and glioblastomas often spread throughout the brain, making surgical removal difficult. Therefore, investigating alternative therapies is essential.
The current team explored an immunotherapy that has previously been overlooked for treating brain cancer: anti-CTLA-4. This immunotherapy blocks cells from synthesizing the CTLA-4 protein, a protein responsible for inhibiting T cell activity. Anti-CTLA-4 was the first available treatment for stimulating the immune system to attack cancer cells; however, it was quickly replaced by the less toxic anti-PD-1.
Due to the quick replacement of anti-CTLA-4 by anti-PD-1 in clinical trials, it was unclear whether anti-CTLA-4 was effective against glioblastoma. However, the clinical trials did indicate that anti-PD-1 was not an effective treatment for this cancer. This encouraged senior author Susan Kaech to explore anti-CTLA-4’s potential.
 Works like a CHARM: the AI model that genomically profiles gliomas
Works like a CHARM: the AI model that genomically profiles gliomas
AI can now offer real-time guidance on how best to remove or treat glioma during surgery.
First, the team trialed both immunotherapies in mice with glioblastoma. After determining that the mice treated with anti-CTLA-4 lived longer than those treated with anti-PD-1, the researchers investigated why.
They found that anti-CTLA-4 treatment caused CD4+ T cells to secrete interferon gamma, a protein that made the tumor release stress signals. CD4+ T cells also alerted microglia, the immune cells of the brain, to the presence of the tumor’s stress signals. This directed the microglia to break down the tumor cells. The microglia then presented broken down fragments of tumor on their surface, encouraging CD4+ T cells to keep producing interferon gamma until the tumor was killed.
“We’re extremely excited to find an immunotherapy regimen that uses the mouse’s own immune cells to fight the brain cancer and leads to considerable shrinkage, and in some cases elimination, of the tumor,” reported Kaech.
In future, the researchers hope to find the same anti-cancer cell cycle in human cases of glioblastoma. Additionally, they plan on examining other forms of glioblastoma in animal models to determine effective treatment plans and to understand glioblastoma better.