Novel CRISPR-based screen identifies target for improved T-cell therapies
Using a new CRISPR-based methodology for modulating DNA structure to enact epigenetic control over specific genes, a team of researchers has identified a “master regulator” gene capable of improving T-cell therapies for treating cancer.
In a recent study, researchers at Duke University (NC, USA) have harnessed CRISPR technologies to help improve T-cell therapies targeting cancer. Their groundbreaking study revealed a “master regulator” called BATF3, which controls the expression of thousands of genes in T cells. This breakthrough has the potential to make T-cell therapies more potent and effective against a wider range of cancer types, potentially opening the door to off-the-shelf treatments and applications in autoimmune disorders.
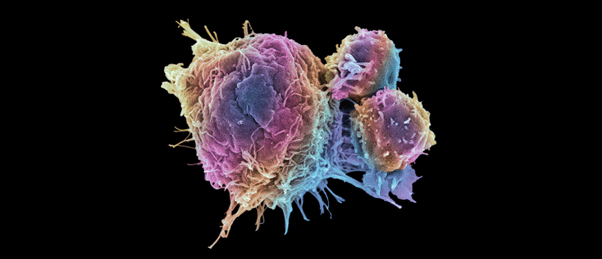
T-cell therapy, which typically involves reprogramming the T cells of a patient’s immune system to seek out and destroy cancerous cells, has emerged as a promising approach to cancer treatment over the past decade. While there have been significant advancements in the field – especially in treating specific leukemias, lymphomas, and multiple myeloma, with a total of six FDA-approved T-cell therapies available – challenges persist when it comes to solid tumors. Solid tumors often present formidable barriers for T cells to overcome, and the sheer volume of cancer cells can lead to T-cell exhaustion, rendering them ineffective.
To address this need, the research team has been working on a method that uses CRISPR-Cas9 to explore and modulate gene expression without cutting the gene. Instead, this approach focuses on modifying the DNA’s structure, a component of epigenetics that impacts gene expression. First author of the paper Sean McCutcheon utilized this method to alter the expression of 120 genes for “master regulators”, proteins that control the expression levels of many other genes, and assessed the impact of these changes on T-cell function.
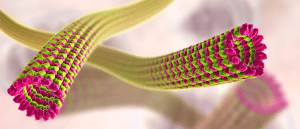 Paralyzing cells could prevent metastasis
Paralyzing cells could prevent metastasis
A mechanism of dynein-powered metastatic locomotion has been identified using soft tissue models, revealing a new clinical target for breast cancer treatment.
The gene BATF3 was identified as a particularly impactful master regulator, the overexpression of which seemed promising for the improvement of T-cell function. To test the potential of BATF3, the team introduced it into T cells and observed that it led to numerous changes to the DNA structure of these cells, resulting in enhanced T-cell potency and resistance to exhaustion.
Testing the potential of this gene further, the team administered T cells engineered to overexpress BATF3 that had been targeted to breast cancer tumors. This approach effectively eliminated the tumors, outperforming the standard of care T-cell therapy.
However, what excites the research team most is the performance of the study’s methodology, which they have demonstrated can be applied to investigate other master regulators to improve therapeutic performance. “This study focused in depth on one particular target identified by these CRISPR screens, but now that Sean and the team have the whole discovery engine up and running, we can do this over and over again for different models and tumor types,” explained senior author Charles Gersbach. “This study suggests many strategies for applying this approach to enhance T-cell therapy, from using a patient’s own T cells to having a bank of generalized T cells for a wide variety of cancers. We hope that these technologies can be generally applicable across all strategies.”
“We are looking for generic solutions that can make these cells better across the board by reprogramming their gene regulation software, rather than rewriting or damaging their genetic hardware,” commented Gersbach. This approach could potentially transform T-cell therapy into a more broadly applicable treatment, improving outcomes for patients with various types of cancer.