Personalization and organoids: On the hunt for rare cancer treatments
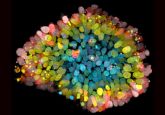
The successful production of patient-derived tumor organoids has provided a personalized approach to treatment options for a selection of rare cancers.
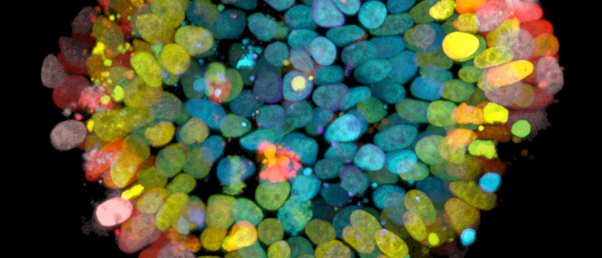
Researchers from the University of California Los Angeles (CA, USA) have optimized a platform to grow tumor replicas – called tumor organoids – using cells biopsied from a patient’s tumor. Using these organoids, the team was able to identify possible treatment options for five patients that previously had few options.
Chordoma tumors are rare bone and cartilage tumors that don’t respond well to chemotherapy or radiation, leaving surgery as the only option. However, when these tumors are in the sacrum or skull base, surgery is complicated, and surgeons often can’t remove the whole tumor. To make matters worse potential new treatment options are further limited by the rarity of sacral chondroma. In cases of rare disease, it is challenging to gather a large enough sample of patients to prove drug efficacy through clinical trials. As such, regulatory approval is difficult.
In this study, the team gathered samples of seven tumors from five patients and created tumor organoids to study the biological characteristics of the cancer and investigate potential therapies. To test the viability of the organoids, the team looked at specific markers for chordoma tumors and found that both brachyury and Ki–67 proteins were expressed in the lab-grown organoids. The group successfully produced viable organoids for all seven sampled tumors, which were then investigated using high-throughput drug screening.
 Steal to survive: pancreatic cancer’s secret to tumor growth
Steal to survive: pancreatic cancer’s secret to tumor growth
Using optical metabolic imaging, researchers find pancreatic cancer cells hijack metabolic activity from non-cancer cells to boost proliferation.
High-throughput drug screening uses automated technology to test enormous numbers of therapeutics on model organisms. In this case, researchers were able to try hundreds of different cancer therapies and assess the reaction of each tumor replica, identifying personalized treatments options.
Interestingly, the study found that each patient produced differing results, despite having the same rare cancer. Furthermore, the study found two tumors from the same patient had differing results.
Looking to the future, lab leader Alice Soragni commented, “Our work continues to be focused on generating individualized models for rare tumors, which often lack therapeutic options, with a long-term goal to leverage these results in the clinic.”
This is the first study that has applied the high-throughput drug screening techniques to patient-derived organoids and makes a powerful argument for the future of personalized medicine in cancer research.