Pick of the posters: AACR 2023
At this year’s meeting of the American Association for Cancer Research (Orlando, FL, USA; 15-19 April 2023), we toured the poster hall, picking our favorites and those most relevant to the members of BioTechniques.
Check out our top 5 poster selections below.
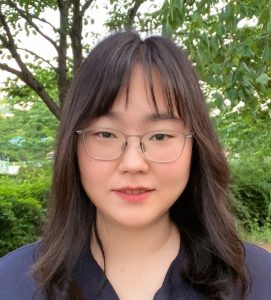
An open-source single-cell spatial image analysis pipeline for 10-plex immunofluorescence of histological prostate cancer tissue sections.
 Jenni Säilä
Jenni Säilä
Doctoral Researcher
University of Helsinki (Finland)
Can you tell us about the imaging technique at the core of this poster?
We are using multiplex fluorescence imaging, staining with 10 different antibodies on a single slide. To achieve this level of multiplex, we do four rounds staining, scanning the image after each round and then combining each of those scans together to generate a 10-plex image in which each of the antibodies feature. This is the first time, to my knowledge, that 10-plex immunofluorescence image analysis has been achieved on a single slide with this level of high throughput image analysis pipeline.
What techniques have you used to subsequently used to analyze these images?
We are using CellProfiler image analysis with ilastik to generate the final results and nucleAlzer to establish nuclear segmentation, then these results are processed with Jupyter Notebook. All of these programs are open source. Then, we are using R programming language to integrate patient registry data into our image analysis and we are doing the data analysis with R analytics.
Do you have any best practice tips for these techniques?
You need to be really thorough when you choose your antibodies, to ensure that they work well with multiplexing. You also need to be really strict with the image curation so that you are able to combine all the images together seamlessly to avoid false positive signals and only measure true signals.
What is one key thing that you want people to take away from your poster?
I want people to see how well you can use this pipeline to stratify different tissues and find localizations of different antibodies and signals. This will allow people to confidently identify where, in the tissue or tumor, different signals are present.
Urine cell-free DNA multi-omics to detect molecular residual disease and predict survival in bladder cancer patients
 Pradeep Singh Chauhan
Pradeep Singh Chauhan
Staff Scientist, Washington University (MO, USA)
Please describe your poster
This poster presents my research into bladder cancer, a multi-omics approach based on urine cell-free DNA analysis to sensitively detect minimal residual disease in urine and predict survival after curative-intent radical cystectomy. In this study, we prospectively profiled urine samples from 74 patients with localized bladder cancer who underwent radical cystectomy, the removal of the bladder and adjacent structures. We integrated ultra-deep targeted sequencing with ultra-low-pass whole genome sequencing (ULP-WGS) to infer three urine cfDNA metrics – maximum Variant Allele Frequency (VAF), inferred tumor mutational burden (iTMB), and tumor fraction level (TFx).
Using a machine learning model, we combined these three urine cfDNA metrics with pretreatment clinical variables and predicted patient survival and response outcomes. The patients who were predicted to be MRD-positive by this model had worse survival compared to patients predicted to be MRD-negative, with comparable performance to gold-standard surgical pathology.
What techniques did you use in this study?
We isolated urine cell-free DNA from these patients and applied two techniques called urine cancer personalized profiling by deep sequencing (uCAPP-Seq) and ultra-low-pass whole genome sequencing (ULP-WGS). uCAPP-Seq is a targeted error-corrected next-generation sequencing technology used to detect mutations at ultra-low levels from urine cell-free DNA. ULP-WGS can be used to infer tumor fraction from cell-free DNA results via genome-wide copy number alteration analysis. Following sequencing analysis of urine cell-free DNA, we performed machine learning with internal cross-validation to predict evidence of MRD after neoadjuvant treatment, which we correlated with gold-standard surgical pathology, and with survival outcomes.
Do you have any tips for best practice when using these techniques?
Both uCAPP-Seq and ULP-WGS are technologies designed to detect tumor DNA from cell-free DNA sequencing. However, both targeted NGS and ULP-WGS are more commonly applied to plasma than to urine cell-free DNA. Additionally, urine cell-free DNA concentrations are quite low in some patients. Thus, we prefer extracting cell-free DNA from at least 25 mL of urine, with EDTA added immediately after collection to preserve stability of the urine cell-free DNA. Other best practices include standard best practices for NGS, sequencing analysis, machine learning, and clinical-correlative analysis.
What’s one thing that you want people to take away from your poster?
Our multi-omic urine-based cell-free DNA analysis allowed for the detection of MRD with high sensitivity and risk-stratified patients by survival. Our technology could form the basis for bladder-sparing treatment in select patients, allowing them to avoid the morbidity of radical cystectomy altogether.
A modified microbiota-accessible carbohydrates diet could change intestinal microbiota in patients with colorectal cancer after surgery
 Boyeon Kim
Boyeon Kim
Cancer Research Institute, Korea University (Seoul, Korea)
Please describe your poster
My poster describes the effect of a high-fiber diet on gut microbiota and metabolites in patients with colorectal cancer. Colorectal cancer patients are advised to consume less than 15g/day of fiber after surgery, but we let them consume 30g/day of fiber. After 3 weeks of a high-fiber diet, beneficial bacteria such as Prevotella, Bifidobacterium and Lactobacillus increased. In addition, short-chain fatty acids, known to be effective in anti-inflammatory, anti-obesity, and anti-cancer indications tended to increase.
Can you tell us about the techniques that you have used to generate the data for this poster?
To analyze the intestinal microbiota, we performed 16S rRNA sequencing of microbes in stool samples from colorectal cancer patients. This was followed by computational analysis using QIIME2 and R programming. In addition, gass chromatography-flame ionization detector and liquid chromatography-triple quadrupole-mass spectrometry were used to analyze metabolites.
What challenges did you face in the production of this poster?
The first challenge was to collect samples from patients as fresh as possible. No matter how good the analysis is, if the sample changes while being transported, it can show different results.
The second challenge was computational analysis. Because the methodology was diverse, it was difficult to determine which analysis was appropriate. It would have been really helpful to have had an integrated website that talks about the techniques used to investigate the microbiome.
If there was one thing that you wanted people to take away from your poster to learn from it, what would that be?
We showed that only 3 weeks on a diet with high fiber can improve the gut microbiome profile. These improvements can lead to better outcomes for patients. For many colorectal patients, it is hard to eat much fiber. However, we want to emphasize that it is important to try to eat a balanced meal with more fiber.
High-throughput 3D tumor models for immunotherapy and drug discovery
 Ryan Smolchek
Ryan Smolchek
Aurita Bioscience (FL, USA)
Please describe your poster
This poster presents a 3D-culture platform we developed based on a cell culture medium we call “Liquid-Like Solids” (LLS), which describes a material comprised of many microscopic solid particles. The intrinsic permeability of LLS enables the convection of both nutrients and waste through the porous network, and conjugation of proteins to the microgel surfaces produces a microenvironment with greater context than base synthetic hydrogels. Here we present several assays we have performed using this platform, including cell migration and immune mediated tumor killing, most of which are facilitated through confocal imaging.
Can you tell us more about the techniques that you have used to generate the data for this poster?
The microgels which comprise LLS physically support tissues and dispersions of immune cells, fibroblasts, ELISA beads, and other samples we work with. However, when acted on by an external force, the particles will flow and behave like a fluid, permitting tools such as pipettes to freely move throughout the medium when composing experiments. This is where liquid-like solids get their name. Self-healing is one of several properties that make setting up experiments in LLS simpler in some respects than other 3D techniques. If we conjugate proteins like collagen to the surfaces of the particles, which cells will use as anchorage points, we can also perform a variety of cellular migration studies.
In this poster we exhibit two example assays, one featuring immune-mediated tumor killing and the other invasion, which quantify cellular motion throughout 3D space. We can then introduce other variables like therapeutics to see if they alter the observed cellular behavior. LLS is essentially water, and the resultant transparency makes it an excellent medium for experiments like these which depend on high-resolution spatiotemporal imaging.
We also use mechanical disaggregation techniques like mincing to break down tumor biopsies and develop them into microtissues roughly 250 µm in size. These samples are highly heterogeneous and recapitulate the enormous complexity present in vivo. Then, we mix these tissues and other samples into the LLS to create the 3D co-culture models we’re interested in studying.
What techniques do you use to analyze these 3D cultures?
Our analysis is largely centered around imaging, using a suite of confocal microscopes to examine different biomarkers and amounts of cytokine secretion. One technique highlighted on our poster is what we call a 3D ELISA bead assay. What we have done is locate ELISA beads in a 3D space around a tumor to study its cytokine concentration profiles. Essentially, the beads fluoresce when interleukin 8 is present, allowing us to quantify cytokine concentration profiles at the tumor margin. This region represents an incredibly small volume, and many other techniques lack the spatial resolution needed to probe it both in situ and in real-time.
Do you have any tips for best practice when generating organoids?
My best tip is don’t ignore the physical properties of the microenvironment. Many culture models result in live cells resting against a stiff substrate that’s generally thousands to millions of times stiffer than what they are used to in vivo. They are likely going to display aberrant behavior which will affect your readout. So, by paying attention to the stiffness you can create a more suitable microenvironment and likely achieve more relevant results.
What’s one key thing that you want people to take away from your poster today?
One key thing: stiffness really matters. We’ve done a lot of studies with different cell lines and always find that even with the same culture media, media exchange frequencies, and densities; making small adjustments to the stiffness in the environment will observably affect their behavior. When you match your 3D culture microenvironment to the relevant physiological stiffness your results are likely to be more relevant.
Evaluating multidrug-resistant genes among breast cancer patients in Ghana.
 Gloria Boaitey
Gloria Boaitey
Kwame Nkrumah University of Science and Technology (Kumasi, Ghana)
What techniques did you use to generate the data for your poster?
We reviewed electronic and manual clinical records of 1,057 breast cancer patients from Komfo Anokye Teaching Hospital (Kumasi, Ghana), which allowed us to establish the prevalence of breast cancer recurrence amongst patients, which has never been done before in Ghana. The prevalence of recurrence was 3.4% and metastasis was 47.6%.
We also took blood samples from 150 breast cancer patients who have been on chemotherapy for at least two years. We carried out single-place genotyping assays to determine the expression of three ABC transporter genes in these women. We are hoping that we can use single-place genotyping assays to predict response to chemotherapy prior to its administration as most women in Ghana have challenges funding breast cancer treatment. If we can know beforehand whether a response will be positive or negative, it will go a long way to improving treatment response and overall survival, which is very low in Ghana and across Africa in most low- and middle-income countries.
When using those assay techniques, do you have any tips for best practice when using them?
For any lab assay, I think the first thing is to make sure you keep the environment clean so that there is no carryover of any contaminant into the samples you are working on.
It is always best practice follow protocols and rigorously document your reagents used and lab conditions so that at the end of the day, once you are done, if another person comes in to repeat the process follows that same protocol, your results will be reproduced.
If there was one thing that you wanted people to take from your poster today, what would that be?
When it comes to women who are diagnosed with breast cancer, those in the developed world often get the opportunity to go through profiling to determine whether they have germline mutations like BRCA1, BRCA2. These screens are not done routinely in Ghana, even though it can go a long way to help in the management of these patients. It is not done routinely because it is expensive and the technology is not available in most hospitals across Ghana.
One thing I would like to say is that when it comes to research in Ghana, we are at a disadvantage due to the technologies that we have available to carry out research, we are behind countries like the USA in this area. Therefore, we need to have collaborations between institutions in low- and middle-income countries and the developed world to bridge that gap, allowing us to conduct research conveniently on location in Ghana, instead of having to travel to other countries seeking help. There should be more opportunities for professional scientists to be trained as I am getting by Cornel Medicine (NY, USA). I think those opportunities should be available to people who are willing to study so that they can take those techniques and skills they have learned back to their home countries to help improve survival in women with breast cancer in their home countries.