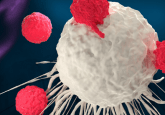
Replacing tired T cells from tumor-draining lymph nodes

Stem-like T cells in lymph nodes serve to replace exhausted T cells in the tumor microenvironment (TME), exposing a new development opportunity for immunotherapies.
A recent study from the Yale Cancer Center (CT, USA), led by Nikhil Joshi, has identified a subset of stem-like T cells in lymph nodes that resupply tumors with active anticancer T cells, helping to bolster the fight against a tumor. The study could have massive implications for the advancement of immunotherapies.
The exhaustion of T cells is a well-observed phenomenon in the TME, whereby an inactive state is induced in the cells by signals released from tumor, allowing it to grow unchallenged. This issue presents a particular challenge for immunotherapies that rely on enhanced T cells, such as CAR-T therapy.
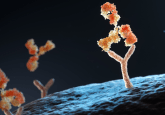
Previous studies have established a positive correlation between the presence of stem-like TCF1+ CD8+ T cells (TSL) in a tumor and outcomes for the patients. These cells stimulate the maintenance of differentiated T-cell populations through the release of the transcription factor TCF1. With this knowledge in mind, the team set out to identify how these cells are maintained in the TME throughout tumor development and avoid the induction of T-cell exhaustion in some instances.
To do this, the team established a mouse model that replicated a developing human lung carcinoma, referred to as the KP model. The tumors in this model can be programmed to start with an immunologically-hot TME, where T cells are active and inflammatory, which develops into an immunologically-cold TME as T cells become exhausted and inactive. This allowed the study of T cells, in both hot and cold TMEs, to examine how they are successfully maintained and what goes wrong to lead to a cold TME.
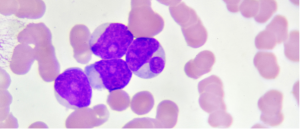 Targeting epigenetics for novel AML treatments
Targeting epigenetics for novel AML treatments
CRISPR screening has identified a new drug target for acute myeloid leukemia, which could lead to the development of a novel therapeutic against the cancer.
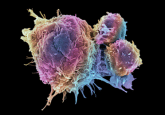
Immunohistochemistry and flow cytometry techniques revealed that even though TSL cells remained present throughout disease progression, the majority of T cells differentiated into exhausted states as the tumor developed and the TME transitioned to a cold state. This indicated that the TSL cells must be resupplied in the TME to ensure their continual presence.
Investigating this hypothesis, the team found that tumor-draining lymph nodes (dLNs) contained similar tumor-specific CD8+ T cells, which were shown to be the developmental precursors of the TSL cells. The dLN T cells were shown to move from the dLNs towards the tumor.
Studying the differentiation of these cells, the team found that while in the lymph nodes, these cells remained undifferentiated, but that their counterparts residing in the tumor were progressively differentiated into an exhausted state. Taken together, these investigations combine to make a strong case for the theory that the levels of TSL cells in the tumor are maintained by a steady supply of fresh dLN T cells.
To establish an element of conservation of this system in humans, the team examined cell samples taken from the LNs of human lung adenocarcinoma patients and found that similar cells were present.
Commenting on the potential impact of the study, first author Kelli Connolly stated that, “this could be an important treatment advance as the potential to respond to immunotherapy is preserved.” Detailing how the team intend to realize this advance, Joshi noted that the team was, “focused on developing therapies that will activate the stem-like T cells in the nearby lymph node and bring them into the fight against cancer. We plan to continue this work and focus on how to improve these therapeutic responses to help patients.”