David Spector: utilizing organoids to study breast cancer
As part of our Spotlight on 3D cell cultures, we spoke to David Spector, Professor at Cold Spring Harbor Laboratory (CSHL; NY, USA) where he is also the Director of Research. David uses 3D cell cultures as a vital tool in his research, using them to identify long-noncoding RNAs of interest in breast cancer and then to screen potential therapeutics for the disease.

What are you currently working on in your lab?
A major focus in my lab is on long noncoding RNAs, which are a very interesting group of molecules. If we look at the human genome, for example, about 34% of annotated genes are protein-coding genes. And yet about 80% of the genome is transcribed. So, we are very interested in this ‘nonprotein coding’ region of the genome. And among the nonprotein coding region, the largest class of genes are long noncoding RNA genes. These represent about 27% of annotated genes in the human genome. We’re interested both in the basic biology of long noncoding RNAs, which are thought to be regulatory molecules, and in trying to identify long noncoding RNAs that play a critical role in breast cancer. Our real motivation is trying to identify new therapeutic targets that can impact disease progression and then identify drugs that can be used to reduce the level of those long noncoding RNAs and help patients.
How do you use 3D cell models in your work?
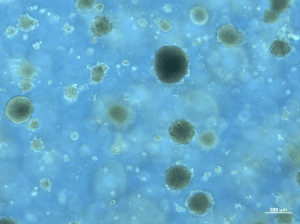
We use them in multiple steps. CSHL has a fantastic strategic alliance with a major healthcare system in the New York metropolitan area called Northwell Health (NY, USA) and I have a protocol in place with several surgeons at Northwell so that I am able to receive fresh patient tumor samples within about two hours of resection from the patient. These are delivered directly to my laboratory. We then take those samples and we develop them into 3D cell cultures, or ‘organoids’. The goal here is twofold; one is to identify long noncoding RNAs that are upregulated in those tumor samples, versus normal samples from the same patient and then a second goal is to use the organoid lines that we’re developing for drug screening approaches.
What challenges do you face in those in the development of those tumor organoids from the tumor samples?
It all comes down to the complexity of disease. Breast Cancer is a very complex disease and we find that organoids we try to make from patients vary greatly in their growth properties, and the ability to passage them over multiple passages in 3D cultures. We do quite well, putting them into the initial culture our take rate is quite high. However, we have great variability once we start passaging them. Some do extremely well, some not so well. It’s not simply related to a tumor grade or a tumor subtype. So, we’re trying to understand what other factors might be playing a role in the ability to keep these lines going for a considerable amount of time.
Once you have that finished product of the tumor organoids, what are some of the key techniques that you utilize with these organoids?
The first thing that we do is fully characterize them. We perform RNA-sequencing analysis, copy number variation, we have a mutation panel that we assess. Then we do some immunohistochemistry looking at Ki67 for example which is a marker of cell proliferation.
Essentially, we’re trying to gain as much knowledge as we can from each of these organoids lines so that we can fully understand their genomic features and output and then how that might impact disease progression.
Do you have any tips for best practice or pitfalls that fellow researchers should look out for when conducting those techniques with 3D cell cultures like organoids?
Right, I think the critical thing that one needs to keep in mind is standardization. This is because the media that is used – and we’re using a medium that was developed at Hans Clevers’ lab (Hubrecht Institute, Utrecht, The Netherlands) – is extremely complex. So we have one person in the lab that focuses on making up the medium that everyone else in the lab is using and that way we can compare data from multiple individuals in the lab. This means we don’t have to worry about slight variability in media contents for various experiments.
When multiple labs are developing organoids, certainly different labs are using different types of media, and one has to always keep in mind that those differences in media composition will certainly lead to changes in gene expression profile. And that will also lead to potential changes in the phenotype. I think standardization in the field is a major area that needs to be paid more attention.
So, are there any ongoing attempts or programs to introduce this standardization into the field of 3D cell culture?
There are a lot of discussions. You know, people are looking at various published protocols and deciding which ones they will use for their particular experiments. It’s not like 2D culture where everybody uses DMEM plus 10% FBS for many different culture types. It’s much more complex. You have to be concerned about the growth factors that you’re adding and the activity of those growth factors when you purchase them from different companies. You can’t be 100% sure that the activity is going to be identical.
These are some of the things that need to get worked out and I know a lot of labs are interested in getting this standardized. I’m sure there are also a number of companies that are trying to play a role in helping to standardize media conditions, etc. I am confident in the long term, just like we buy DMEM, there will be commercial products that will be worked out that are standard. That would be a great thing to see.
With the complexity of the media evolved, does that also bring challenges with contamination?
Fortunately, we don’t have any contamination issues in our lab, but it is something that we are quite neurotic about. We do all of our culture work in laminar flow hoods, the incubators that we use are only for organoids, we have a separate room where we do our organoid only culturing; we don’t allow anyone to bring, for example, mouse cells or HeLa cells into that room. We are just very careful and we try to control things as best we can.
When utilizing tumor organoids in your research, how do they compare to animal models in your studies? What are the pros and cons of the two?
No one system is the one and only. You can learn things from many different systems and I think that’s the best approach. You learn a lot from 2D culture but you don’t learn everything, and it’s similar with organoids. I don’t think that organoids are going to totally replace mouse models. They certainly add a significant capability. But we still do mouse experiments in my lab and we try to glean what information we can from the mouse or human organoid models and in some cases even some 2D culture. We bring all that information together to develop our research goals.
The big advantage of organoids is that these are true patient samples, which are extremely valuable. In terms of our studies and in terms of long-term costs, I think organoids have a big advantage over mouse models. Keeping huge mouse colonies going is more expensive and labor intensive.
Organoid models are more scalable as well because we can have 50 different patient samples, which we have a biobank of. We can ask our question many times and under different experimental conditions using the samples from this biobank. We couldn’t do that in a large number of different mouse models. It would be impractical.
Can you identify any discoveries that tumor organoids have facilitated that you wouldn’t have been able to uncover had you just been using animal models?
With 3D organoids, we have the ability to identify long noncoding RNAs that are upregulated in breast tumors versus normal mammary epithelial cells from the same patient, as they are derived from patient samples. So we have, in a sense, the perfect control. We’re not just pulling out some normal cell line and comparing it to our tumor cell line. We’re taking material from the same patient and doing comparative studies. I think that’s extremely valuable.
It has allowed us to identify some long noncoding RNAs that are upregulated in tumors. And we’re currently working on them to try to understand their molecular function.
Do you have any idea, as of yet, what the molecular function of those identified, long noncoding RNAs could be?
So, we’re very early in our studies there but we have an interesting story. In one case, we initially start working on a long noncoding RNA, in our mouse models. Then we identified the human ortholog, and then pursued it in our patients’ tumor organoids. We then did a comparator to see how well-conserved function is for this long noncoding RNA between mouse and human.
A really cool experiment that we did was to knock out the mouse gene for this particular long noncoding RNA and then after identifying the human ortholog – identified by synteny, not by sequence identity because long noncoding RNAs tend to not necessarily be conserved by sequence but more by synteny – we cloned the human ortholog. We then expressed it in our mouse knockout cells and showed that we could rescue the phenotype. Thereby, clearly demonstrating that it was in fact, the human ortholog. We are now assessing its function in our human patient-derived breast tumor organoids
What do you most enjoy about working with organoids?
The fact that we’re working on samples that are as representative as we can get to evaluating a patient’s tumor, and are then able to manipulate that sample in ways that might provide an insight that could potentially help the patient, is really exciting. The ultimate goal here is to be able to take a tumor sample from a patient, put it into 3D culture and then treat it with a battery of different drug combinations and identify in a patient-specific manner what might be the best drug combination or drug for that particular patient.
If there was one aspect of working with organoid models that you could ask for to be improved, what would it be?
Right now, we need better methods for making knockouts and for tagging various molecules in the organoids. That would be a huge help for our particular work. Also, as I said earlier on, even better optimizations of the growth medium. I think there’s still work that could be done there.
Is this an area that CRISPR could begin to assist in as it develops or are there other techniques that you think you would employ?
I think getting the CRISPR methods to work efficiently in organoids would be a huge plus. We’re currently taking a different approach. Just to get around the fact that methodology is not yet optimized in organoids. We’re using antisense molecules that can knock down particular RNAs. We find in many of our organoid lines that we can achieve about a 95% knockdown using antisense oligonucleotides.
We have a very strong collaboration with a pharmaceutical company (Ionis Pharmaceuticals, CA, USA) that works with us to design these molecules that we can use in organoid lines to assess the impact of knockouts on these systems.
If you had any advice for early career researchers, what would that advice be?
Come up with important innovative questions and innovative approaches to address those questions. Use a wide array of approaches to address your question. Think about the potential impact of what your work will have on your field,
Where would you predict the field of organoid and 3D cell cultures could progress to in the next 5 years.
In the next five years, I think we’ll get closer to moving these systems towards being able to impact clinical decisions. I mean we’re already starting to move in that direction. And so I would expect that would be a very significant and impactful development.
At CSHL, we have established an organoid facility. The hope is that will strengthen our clinical collaborations. We plan to have part of that facility, set up as a CLIA certified lab that would have the ability to provide insights back to clinicians.





