Two minutes with: Manel Esteller on the epigenetic validation of cancer organoids
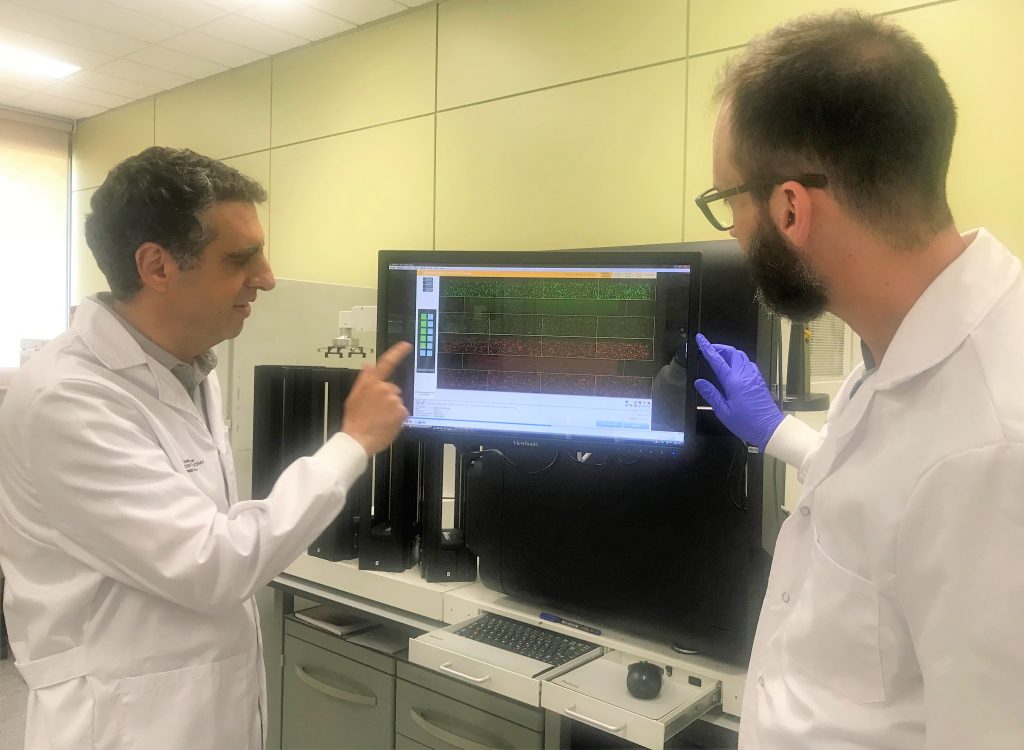
Tasked with mapping the epigenetic landscape of human cancer organoids from the Human Cancer Models Initiative, Manel Esteller (Josep Carreras Leukaemia Research Institute, Barcelona, Spain) set out to provide information on the DNA methylation profiles of human cancer organoids. In this interview, Manel outlines the critical need for 3D models for cancer to be validated and, therefore, more prevalent in cancer research, and documents the key findings from his recently published paper in Epigenetics.

Please introduce yourself and your institution.
I am Dr. Manel Esteller, Director of the Josep Carreras Leukaemia Research Institute (IJC), Chairman of Genetics in the School of Medicine of the University of Barcelona, and an ICREA Research Professor. For many years my lab has studied the alterations in DNA methylation, histone modifications and chromatin that occur in human disease, particularly in cancer. We are also interested in finding epigenetic biomarkers in precision medicine and the development of new epigenetic drugs.
Can you tell us about the organoids that you examined in your recent study?
Most of the discoveries in cancer research are derived from two types of samples: the primary tumors removed from surgical procedures from the patients and cancer cells that grow in the lab within plastic flasks called cell cultures. These systems both have caveats: primary tumors have a shortage of biological material and cannot be maintained for extended periods of time, whereas the cell lines grown in the lab are not dividing in their usual surroundings and only grow in 2D, far from their natural conformation. That motivated us to assess if a third model was able to better mimic the real tumors, driving us to determine the value of these cancer systems called organoids.
What techniques did you use to study the cancer organoids?
We used genomic material purified from cancer organoids to determine the profiles of chemical modifications that took place in the DNA. Our DNA is a combination of four bases adenine, thymine, cytosine and guanine (or ATCG) in 6,000 million nucleotides. We specifically targeted DNA methylation – the addition of a methyl group (CH3) to the C. This mark acts as a ‘stop traffic signal’, repressing the activation of the underlying gene. We used a comprehensive DNA methylation microarray approach to analyze close to 1 million sites of DNA methylation changes, thus combining genomic and bioinformatic approaches.
What were some of the most exciting discoveries that you made in this study?
Three bodies of data of particular interest can be highlighted. According to epigenetics, the organoids really looked-like the tumor types of the surgical specimen, i.e. the colon cancer organoid mimicked a colon cancer biopsy. The cancer organoids did not contain contaminating healthy cells, thus the transformed cells can be studied in a purer manner; and finally, the cancer organoids resembled the real tumors obtained from the surgeries of oncology patients more than the long-established 2D cancer cell cultures grown in plastic flasks in the lab.
Epigenetics with Manel Esteller
In this BioTechniques behind the technique, we met Manel Esteller – Director and Group Leader at the Josep Carreras Institute (Spain) – at AACR 2019 to discuss the importance of epigenetics in cancer research, the best techniques for studying epigenetics, as well as his research focuses and where he thinks the field of epigenetics will head in the future.
What are the implications of this study on the use of these cancer organoids in drug development?
Some promising cancer therapies fail when applied to clinical settings despite showing promise in the preclinical studies. Most of these agents show their efficacy first in 2D cancer models in labs, whereas the real tumors are 3D. The use of 3D organoids can help to overcome this problem. Our study proves that organoids are valuable systems to test the efficacy of drugs targeting cancer cells, not the surrounding environment. They can be assessed for DNA damaging agents, tyrosine-kinase inhibitors or microtubule targeting for example. And the efficacy can be quickly characterized by cell death or growth inhibition common tests. Cancer organoids can enhance preclinical drug development and augment the likelihood of success for later trials in medical oncology.
What aspects of these organoids do you think need to be improved in order to make them even more representative of in vivo tumors.
We would love to expand our discoveries to obtain the epigenetic landscape of human cancer organoids for other cancer types not initially included in the study, such as breast, lymphoma and brain cancer. We would also like to determine how the epigenetic landscape of cancer organoids change if they are co-cultured with immune cells, another exciting area in cancer research. If we also add other cell types such as fibroblasts and endothelial cells, then we have a cellular mixture that might look almost identical to the tumor inside the body of the patient. I believe that organoids could become a very useful tool to predict drug responses to cancer drugs in a timely and cost-effective fashion.
