Exploring platelet-induced metastasis with organ-on-a-chip technology

The mechanism driving the interaction between platelets and cancer cells, which stimulates metastasis, has been revealed with a new organ-on-a-chip model.
A novel organ-on-a-chip model, the ovarian tumor microenvironment chip (OTME-Chip), has been developed by researchers at the Texas A&M University (TX, USA), led by Abhishek Jain. The model has successfully revealed the mechanism through which platelets promote the metastasis of ovarian tumors, highlighting a novel drug target to bolster the success of chemotherapies.
The research team set out to explore platelet extravasation into the tumor microenvironment (TME) and how tumor metastasis is accelerated by the infusion of blood cells. It is also understood that platelet extravasation can aid tumors in their resistance to chemotherapy.
To investigate this process, the team first selected a cancer type for their study that is renowned for its rapid spread and the challenging nature of its observation: ovarian cancer.
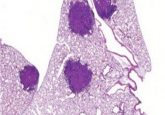
Jain constructed an organ-on-a-chip model with two compartments, stacked one on top of the other. The top compartment consisted of a tumor chamber containing epithelial ovarian cancer cells, flanked on either side by extracellular matrix (ECM) chambers; the bottom compartment, one vascular chamber lined with ovarian microvascular endothelial cells. The two compartments were separated by a matrix-coated polydimethylsiloxane (PDMS) membrane, while PDMS micropillars separated the three chambers of the top compartment.
 Exposing the super enhancers behind breast cancers
Exposing the super enhancers behind breast cancers
A recent multiomic study has established a super-enhancer-target regulatory network for breast cancers, exposing new epigenetic targets for therapeutics, particularly in triple-negative breast cancer (TNBC).
This model allowed the team to pass a solution of platelet cells through the vascular chamber, observing as the platelets perfused through the PDMS membrane into the tumor chamber over the course of three days. The team used high-resolution fluorescence imaging and confocal scans to observe the perfusion and the subsequent invasion of the cancer cells from the tumor chamber into the ECM chambers.
Subsequent analysis using advanced cell and molecular readouts, gene-edited tumor cells and RNA sequencing methods in combination with the OTME-Chip granted the team unparalleled insight into the interaction of ovarian tumor cells and platelets. “…We discovered the actual genetic signaling pathways behind the blood cell triggered metastasis of ovarian cancer and a new drug strategy to stop this process,” noted Jain, highlighting the value of the OTME-Chip.
The mechanism uncovered relies on the platelet surface receptor GPVI interacting with the tumor cell surface glycoprotein galectin-3, leading to the upregulation of a sequence of growth factors that promote metastasis. With this knowledge in hand, the team tested the effects of the GPVI inhibitor Revacept on the system. The tumor’s metastatic potential was reduced and the impact of chemotherapy increased on the administration of the drug.
The team is confident that this tool can now provide researchers with a perceptive tool with which to identify novel drug targets and further understand cancer. “This multimodal OTME-Chip is going to provide an ideal platform to the health care researchers to evaluate their anti-cancer, vascular and hematological drugs individually or in combination in an artificially created human-level tumor microenvironment,” concluded Jain.