Application Note: Antibody–drug conjugates: a novel paradigm for cancer therapy
Chemotherapy is one of the most widely used cancer therapies; however, chemotherapy often causes serious side effects. Antibody-drug conjugates (ADCs) are promising emergent cancer therapies that combine the effective killing power of small molecule cytotoxins and the highly specific targeting ability of monoclonal antibodies (mAbs). Thus, ADCs precisely deliver cytotoxins to tumor cells, while minimally affecting normal cells. ADCs have become a hot spot for anticancer drug development [1,2].
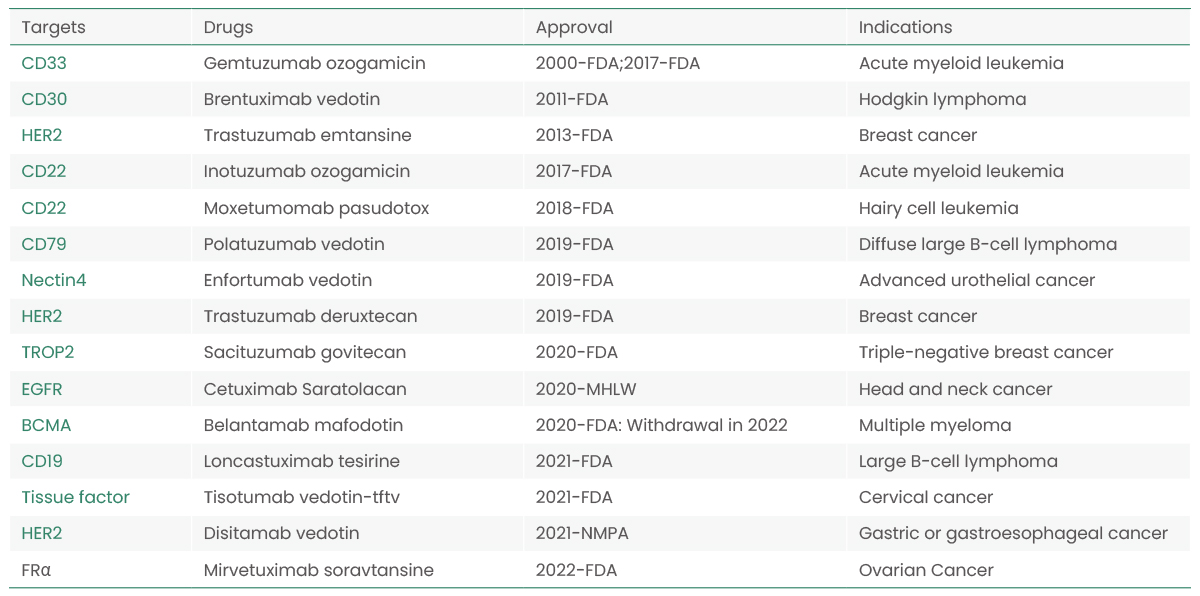
The first-generation ADC, gemtuzumab ozogamicin, was approved by the U.S. Food and Drug Administration (FDA) in 2000. Since then, multiple ADCs have been approved worldwide, and more than 100 ADC candidates have entered the clinical phase. These new anticancer drugs are leading the way to a new cancer therapy phase.
Table.1 Currently approved ADCs on the market.
Key Components of ADCs
An ADC consists of a target-specific mAb, a cytotoxic payload, and a chemically synthesized linker that covalently links the toxin and the antibody. The mAb binds to specific antigens on the surface of tumor cells, and ADCs are internalized into tumor cells during the formation of antibody-antigen complexes. ADCs are typically transported from the endosome to the lysosome, where the linker is cleaved and the small molecule cytotoxins are released, leading to tumor cell death [3]. Overall, ADC development requires consideration of the target antigens, antibodies, cytotoxic payload, and linker (Figure 1).
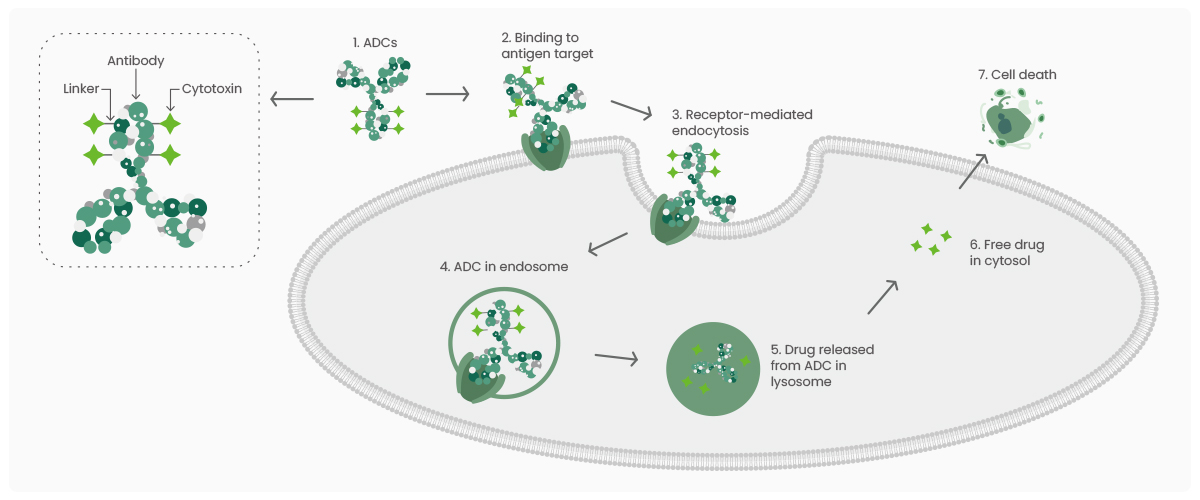
Figure 1. The general mechanism of action for antibody-drug conjugates (ADCs).
Target Antigens
Target antigens should be non-secretory, expressed mainly on the tumor cell surface and expressed at low levels in normal tissues. In addition, target antigens should be internalized after binding to the corresponding antibodies to facilitate the entry of ADC-antigen complexes into tumor cells to release cytotoxic payloads via an appropriate intracellular translocation route [4].
At present, the target antigens for approved ADC drugs are specific proteins overexpressed in tumor cells, including HER2, Trop2, Nectin4, and EGFR in solid tumors, and CD19, CD22, CD33, CD30, BCMA, and CD79 in hematologic malignancies. Emerging targets, such as EpCAM, CD70, CD25, CD166, and others, are under development and showing promising results [5]. Sino Biological is at the forefront of the ADC therapy field, providing quality products for ADC target antigens.
(a)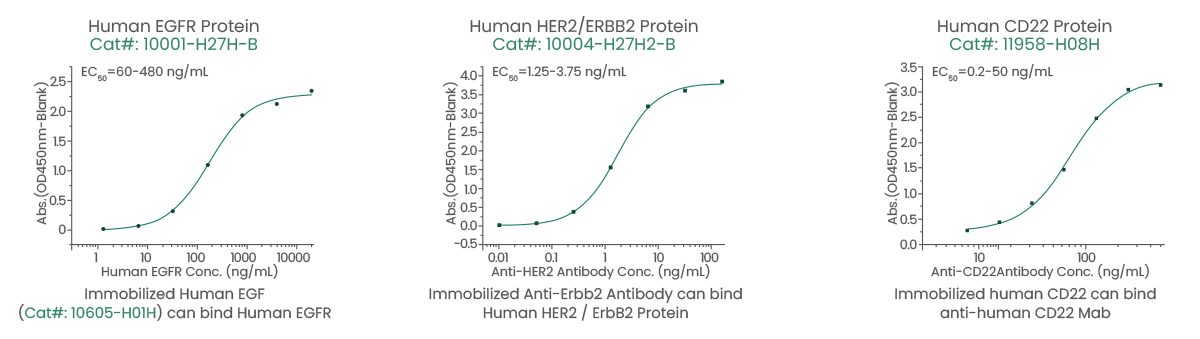
(b)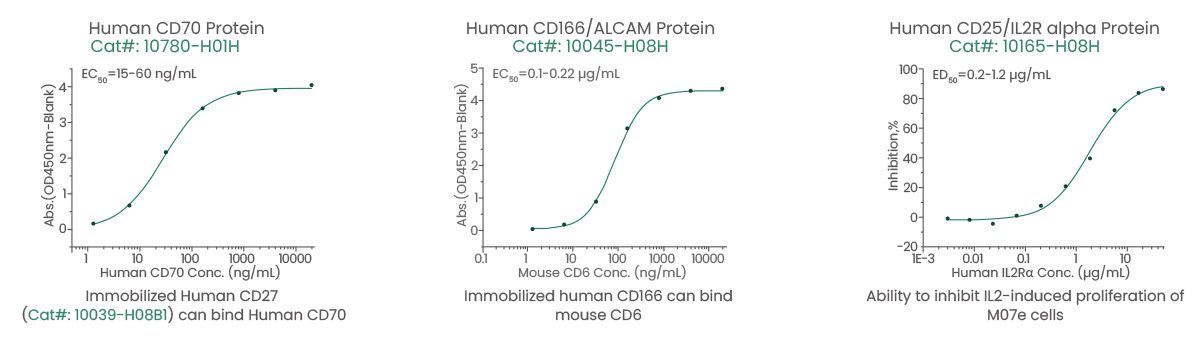
Figure 2. High-quality target antigen products. (a) Well-established targets: EGFR, HER2, and CD22. (b) Emerging targets: CD70, CD166, and CD25.
Antibodies
Immunoglobulins (IgGs) and their derivatives are commonly used in clinical studies. IgG1, IgG2, and IgG4 are mainly used for ADCs because of their specificity, affinity for the target antigen, and long circulating half-life. In addition, the antibodies should possess effective internalization ability and low immunogenicity[6].
In early ADC drug development, predominantly mouse antibodies were used. However, these antibodies elicited a significant immune response, resulting in reduced therapeutic efficacy. With the advent of recombinant technology, mouse antibodies have been replaced with chimeric and humanized antibodies. Currently, ADCs increasingly use fully humanized antibodies with significantly lower immunogenicity [7].
Sino Biological provides high-quality mAb humanization services using complementarity-determining region (CDR) grafting technology and computer-aided molecular modeling. In addition, Sino Biological possesses the high-throughput and scale-up capabilities to produce highly efficient antibodies in HEK293 and CHO cells in as fast as 2 weeks, with over 1000 Abs expression per batch.
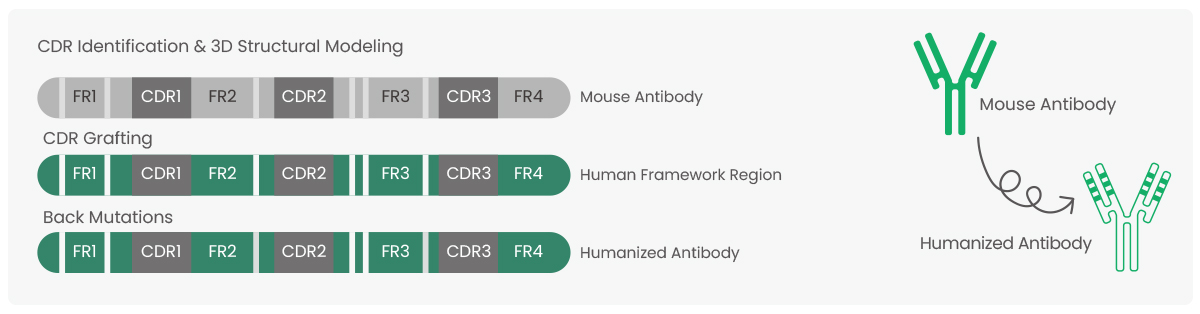
Figure 3. The process of antibody humanization and complementarity-determining region (CDR) grafting technology.
Cytotoxic Payload
Cytotoxins should have high toxicity, low immunogenicity, and high stability. In addition, the cytotoxin should have a modifiable functional group or a site where a functional group can be introduced to link the mAb. The most commonly used cytotoxins for ADC drugs on the market or in clinical trials are microtubule protein inhibitors or DNA-damaging agents [8]. Additionally, the drug-antibody ratio (DAR), i.e. the number of drug molecules attached to the antibody by the linker, is a key factor in ADC development. A low DAR may reduce ADC efficacy, while a high DAR may cause instability, leading to off-target toxicity [8,9].
Linker
The linker ensures that the cytotoxic payload remains firmly attached to the antibody in the plasma during circulation, avoiding premature release that would damage normal tissues or cells and ensuring the effective release within the target tumor cells. Linkers can be classified as cleavable and non-cleavable. Cleavable linkers take advantage of the environmental differences between the circulation and tumor cells to accurately release free cytotoxins. Non-cleavable linkers depend on lysosomal degradation of the entire antibody-linker structure, which results in the retention of charged amino acids in the payload [10,11].
Challenges and Perspectives
Many challenges remain in ADC development. The biggest challenge is the toxic effects of ADCs, including neutropenia, thrombocytopenia, leukopenia, anemia, and gastrointestinal effects [4]. Another challenge is tumor resistance to ADCs, as evidenced by reduced antigen expression levels, altered intracellular transport pathways, and payload resistance. In addition, payload release is a challenge. The ADCs are much larger than traditional cytotoxic drugs, and the efficiency of cytotoxin penetration into tumors is limited.
To overcome these challenges, future ADC development should focus on the following: improvements in ADC design to reduce toxicity, including payload platforms, linkers, and coupling strategies; use of two cytotoxic agents as payloads to reduce ADC resistance; and enhancing ADC internalization and lysosomal delivery through bispecific antibodies to improve antitumor specificity. Sino Biological utilizes an optimized mammalian cell expression platform to provide fast and efficient bispecific antibody expression services for clients worldwide [12].
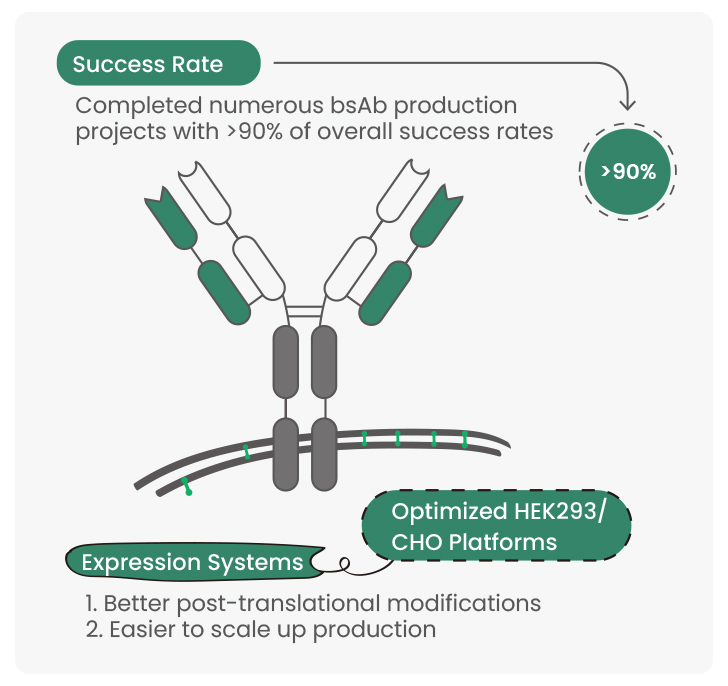
Figure 4. Sino Biological bispecific antibody production service highlights.
ADC therapy has benefited many cancer patients. In the future, the therapeutic efficacy of ADC will be improved by reducing ADC toxicity and drug resistance. Sino Biological will continue to be at the forefront of the ADC therapy field, providing researchers and pharmaceutical companies with high-quality products and one-stop services.
This content was provided by
