Why do some AML patients respond better to immunotherapy?
Immune cells in the bone marrow microenvironment of AML patients are key in distinguishing a response to immunotherapy.
A team of researchers from Colombia Engineering and Irving Institute for Cancer Dynamics (both NY, USA) have identified a distinct T-cell population in relapsed acute myeloid leukemia (AML) patients that play a vital role in an effective response to immunotherapy. They also identified key characteristics of a recipient’s bone marrow microenvironment that could be predictive of a positive response. These findings offer insights into potential improvements to immunotherapy approaches.
Currently, the standard treatment for AML is targeted chemotherapy followed by hematopoietic stem cell transplantation (HSCT). However, the rate of relapse after HSCT remains high at 40%. Upon relapse, the only way to treat AML is to restore immunological control through donor lymphocyte infusion (DLI), a type of immunotherapy for which the response rate is only 15-20%. The specific cell types and mechanisms that influence response or resistance to DLI are still unclear.
The team previously identified that expansion of precursor-exhausted T cells is a key feature in determining response to DLI in chronic myeloid leukemia patients, yet it remains unknown if this population is also associated with response to DLI in AML patients. Therefore, the team aimed to characterize cellular crosstalk in the bone marrow microenvironment of relapsed AML patients treated with DLI, to gather insights into the factors that determine immunological response or resistance.
The team profiled bone marrow mononuclear cells by performing single-cell RNA sequencing, single-cell T-cell receptor sequencing and cellular indexing of transcriptomes and epitopes by sequencing (scCITE-seq) for proteomic characterization. To further characterize cellular crosstalk in the bone marrow microenvironment the team applied their new Bayesian model approach, DIISCO, followed by spatial confirmation by CODEX.
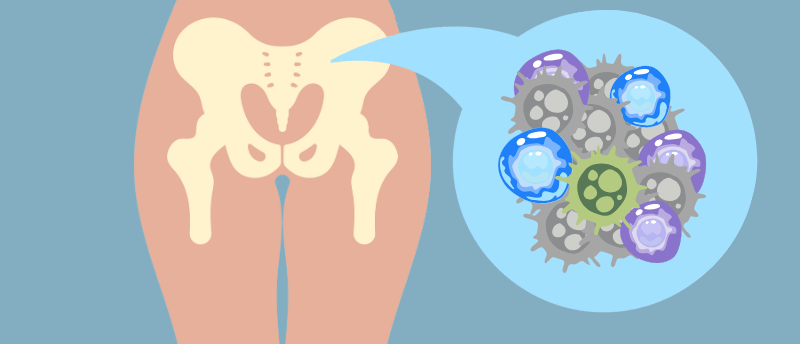
AML patients who responded to DLI were found to have a higher diversity of immune cells in their bone marrow microenvironment prior to DLI. This diversity was found to increase over time post DLI. These immune cells interacted and coordinated to create a network of activity that promoted T cell effector activity, which is central to DLI response. Conversely, AML patients who did not respond to DLI were found to have a lower diversity of immune cells and a dominance of myeloid cells in the bone marrow microenvironment.
The team demonstrated that after DLI these highly diverse immune populations converged upon CD8+ZNF683hi cytotoxic T cells (CTCs), which have direct antileukemia activity, marking this T-cell population as a distinguishing feature in a positive DLI response. Those who did not respond to DLI had lower levels of CD8+ZNF683hi CTCs and instead had higher levels of inhibitory marker-expressing CTCs.
CD8+ZNF683hi CTCs were found to have originated from the DLI product, however, their activation and expansion is dependent on the recipient’s bone marrow microenvironment, favoring those that are more diverse and less immune inhibitory.
“Our findings not only shed light on mechanisms underlying successful immunotherapy response in leukemia but also provide a roadmap for developing effective treatments guided by innovative machine learning tools.” commented study lead Elham Aziz.
The team plans to continue their research into methods of enhancing the effectiveness of DLI through modulating the tumor microenvironment.