Heart organoid model illuminates key aspect of congenital heart defect pathology
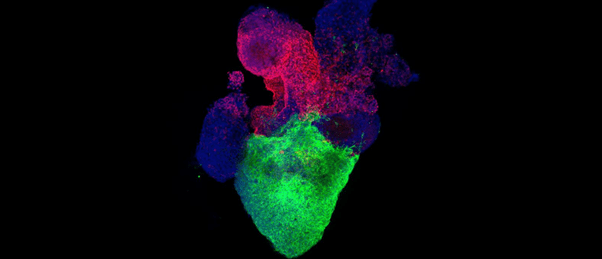
An organoid model of the human heart provides insights into the pathology of diabetes-induced heart defects in newborns.
Researchers from Michigan State University (MI, USA) have used human heart organoid technology to study the link between pregestational diabetes and congenital heart defects in greater detail.
Congenital heart defects are the most common newborn defect. Pregestational diabetes (PGD), diabetes which affects the mother before or during the first 3 months of pregnancy, is associated with an up to 12-fold increased risk of congenital heart disease for the newborn child.
Studying congenital heart disease is difficult due to an overreliance on animal models. Those animal models that are available, predominately rodent, differ significantly in terms of cardiac physiology, electrophysiology and of course the actual size of the heart.
In a recently published paper, researchers describe how they have used an organoid model to recapitulate the conditions seen in the developing heart of fetuses whose mothers have PGD.
The team began modeling PGD conditions by exposing their organoid model to a high-glucose and high-insulin medium (a hyperglycemic environment). They observed that organoids in this medium exhibited cardiomyocyte hypertrophy, a key initial feature of PGD-induced congenital heart disease. Through mitochondrial staining, they also detected swelling of the mitochondria and abnormalities in their morphology.
 Researchers develop new heart organoid
Researchers develop new heart organoid
Researchers have created a heart organoid containing both cardiomyocytes and epicardium for the first time.
Additionally, increased cellular reactive oxygen species (ROS), less organized vascularization and a higher frequency of arrhythmic events were seen in the organoids exposed to the hyperglycemic conditions. Overall, these match up with the pathological hallmarks of PGD-induced congenital heart disease that have been previously reported in humans and mice.
Delving deeper into the higher levels of ROS, the team found these were centralized to the endoplasmic reticulum (ER), resulting in ER stress. Using single-cell RNA sequencing, the team discovered that a combination of ER stress and lipid imbalance drive diabetic embryonic cardiomyopathy, which was confirmed using imaging and lipidomics.
To investigate whether restoring the lipid balance and reducing ER stress could mitigate the harmful effects of PGD in the heart organoids, the team tested potentially therapeutic strategies, including introducing a mixture of omega-3 fatty acids to the organoid medium and targeting inositol-requiring enzyme 1 (IRE1). By doing so, the effects of PGD were partially reversed. From this, the researchers hypothesize that providing diabetic mothers with a dietary supplementation of omega-3 fatty acids during the first 3 months of pregnancy may be a possible way to prevent the early stages and development of PGD-induced congenital heart disease.
Speaking on next steps for the study, senior author Aitor Aguirre noted: “On one hand, we want to partner with clinicians to establish the efficacy and safety of our findings in pregnant women. On the other hand, we want to apply our organoid model to other conditions affecting congenital heart disease so we can improve the lives of these children in the future.”