Examining endotoxin contamination for improved 3D cell cultures
 Jai Prakash (left) is a Professor in the Department of Advanced Organ Bioengineering and Therapeutics at the University of Twente (Enschede, Netherlands), where he works with Postdoc Marcel Heinrich (right) on the development of engineered therapeutics targeting the tumor microenvironment (TME) using 3D in vitro models.
Jai Prakash (left) is a Professor in the Department of Advanced Organ Bioengineering and Therapeutics at the University of Twente (Enschede, Netherlands), where he works with Postdoc Marcel Heinrich (right) on the development of engineered therapeutics targeting the tumor microenvironment (TME) using 3D in vitro models.

In their pursuit of improved models through which to design more effective cancer therapeutics, the pair have come up against the issue of endotoxin contamination in 3D cultures and have made it their mission to resolve this plight on the development of effective, reproducible 3D cultures. Here, they discuss this issue and their efforts to resolve it.
Can you give us an overview of your lab’s focus?
Jai: My lab is focused on the development of new therapeutics targeted to the TME. Tumors are not just composed of tumor cells there are a lot of different cells that interact with each other both within and surrounding the tumor. The last 10 years have been transformational for our understanding of tumors’ interactions with their immediate surroundings and how they create an environment that is favorable to their growth: the TME. Our aim is to target specific cells of the TME in order to inhibit their function and stop them supporting tumor cells.
During this process, we have determined that we need to have better 3D models to replicate this environment. Previously, when focusing on tumor cells, it was fairly simple: you took the tumor cells, tested the therapy on them and monitored their response. But if you want to study an environment where a number of cells are interacting with each other, then you need a model that replicates that complexity. In the last 5 or 6 years, as technologies have developed, we have been able to generate 3D models composed of multiple different cell types in order to study the interactions of cells in the TME and test the therapeutics we develop.
What are some of the challenges in establishing effective 3D cell cultures?
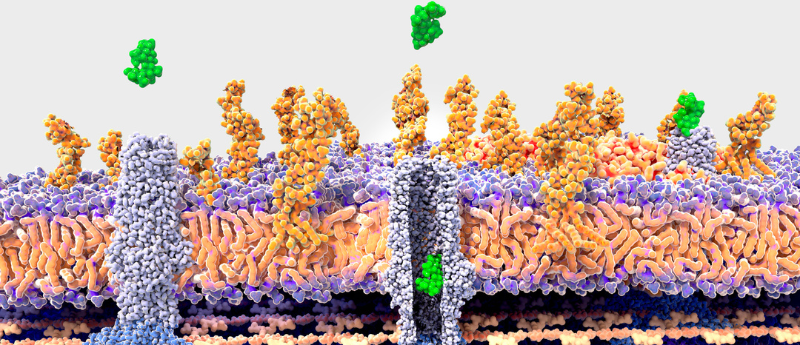
Marcel: If you look at a 3D cell culture, there are essentially two components. The first is the cells and the second is the matrix that provides them with the 3D shape. There are some models that rely solely on the cells to produce this matrix, called spheroids, but most models now utilize synthetic matrices.
The matrix component poses a big challenge because it needs to be tissue-specific, it should mimic sections of the tissue that you want to recreate and its composition must be well-controlled. To get this control, the material itself needs to be very tunable so you can tune it to the precise indication or tissue you want to study. The aim is to provide the cells with the optimal surrounding for interactions to other cells, allowing them to proliferate and communicate, but without the material itself interfering in the process; the cells should be able to self-direct and differentiate based on their own cues as opposed to stimuli from the matrix. What’s more, the matrix must be highly reproducible, especially if we use these models to test and compare a number of drugs. We need models that are identical each time we produce them.
So, we are asking a lot from this material and the slightest disruption can disturb the delicate balance that you are trying to strike. This is how we came to focus on the issue of endotoxin contamination.
What are endotoxins and how can they interfere with the generation of effective organoids?
Marcel: In general endotoxins are part of the bacterial cell wall. They bind to a specific receptor, TLR4, on human immune cells and can cause severe immune reactions, such as inflammation, which can lead to septic shock in extreme cases. Recently it has been shown that a lot of other, non-immune cells also have this receptor and can be affected by endotoxins. For instance, there’s some evidence now that endotoxin contamination can delay bone and skin regeneration.
In the TME models that we make, we focus on immune cells and often test immunotherapies with them. As you can imagine, a matrix or a model that contains endotoxins will stimulate an inflammatory response from the immune cells, and eventually, the whole model is biased from the beginning. It will display an inflammatory readout regardless of the cells you test with it or the therapies you challenge it with.
For example, in tumors, the macrophages, a prominent cell type in the TME, are often anti-inflammatory to suppress the immune environment. But if you have a model that is inherently inflammatory, then you have failed to accurately replicate the environment of an in vivo tumor.
How are you working to overcome this challenge?
Jai: You need very high-quality materials to prevent this. Currently, there are a number of new players in the market selling these biomaterials for research purposes. But when you buy this material, you don’t know its quality and unfortunately, the contamination of endotoxins is very difficult to detect. The assays we currently have available for endotoxins are not very good. What we need is for suppliers to guarantee high-quality materials accompanied by a certificate that gives you a full view of the contamination.
The second thing I think we need is for journals to specifically ask authors to provide information about endotoxin analysis. If the journals demand this specification, researchers will automatically ask their supplier or will test their materials themselves before even starting their research. I think this chain reaction is what’s needed for us to move forward. We are taking care from our research that we work with materials that have been fully certified and tested well.
How have you been working with suppliers to improve your work and the standards and materials they’re providing?
Jai: We have worked with a company called Rousselot, which is capable of extracting endotoxins out of their biomaterials and so can provide high-quality material. Rousselot provided the support we needed to facilitate comprehensive testing of the quality of various biomaterials and to enable us to fully investigate the impact of endotoxins on 3D models for new therapeutic research and development.
It is very difficult to receive this level of support for studies that focus on improving reproducibility and experimental rigor, or characterizing endotoxins! On the surface, this might appear to be relatively low impact or unexciting for new research, but yet it is really important and we need to bring attention to it.
If there was one thing that you could ask for to improve the establishment of 3D cell cultures, what would it be?
Jai: I think one key problem for 3D models is the matrix and selecting the correct biomaterial for different purposes. There won’t be one material that fits all our needs, it will be a specific material for a specific tissue. What I would like is for the community to form a consensus on which material to use for each tissue, both healthy and diseased, and to have that information freely available and well observed.
Marcel: I agree with Jai. Collagen or gelatin are the gold standards for cell culture; however, the mechanical properties of brain or breast tissue are different. So, if we could have a wide portfolio of collagen and gelatin with different mechanical properties to create the best fit for each tissue, that would be helpful. What would be fantastic is if you could buy these specific materials off the shelf, for instance, a “matrix of the brain” that has all the extracellular matrix components that you need to make a representative brain culture. At the moment it is self-directed assembly, which is going to lead to different results in different labs.