New organoid model mirrors microglia development
A novel method involving the xenotransplantation of cortical organoids has facilitated fascinating new insights into the development and function of microglia.
A recent international collaboration, led by senior author Rusty Gage (The Salk Institute, CA, USA), has developed a novel approach for establishing brain (or cortical) organoids that can sustain microglia and be xenotransplanted into living animal models for in vivo investigations. This platform provides a more authentic environment for the examination of microglia, a famously difficult-to-study cell type, and their interactions as they proved in an investigation of macrocephalic autism spectrum disorder that yielded some interesting results.
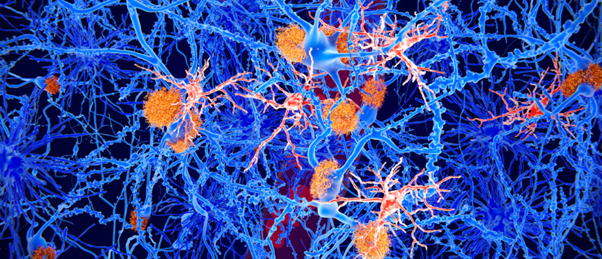
Microglia are specialized immune cells localized to the brain, which mediate neuronal development, maintenance and repair. While their importance is well recognized, these cells “lose almost all function and meaning,” when removed from the brain environment, according to Gage. Organoid models have been developed for the study of microglia, but challenges with vascularization, lifespan and sustaining cellular heterogeneity have meant that these cells remain difficult to study and our understanding of their function and interactions is limited.
To overcome these challenges, the team colonized cortical organoids with human-stem-cell-derived erythromyeloid progenitors (EMPs). These cells are the precursors from which microglia develop. Once colonized, they engrafted the organoids into the retro-splenial cortex of immunocompromised mice. This enabled vascularization of the grafted organoid, which led to the maturation of the EMPs into functionally mature human myeloid cells that survived long term within the organoid but did not spread to the host.
This living, in vivo model of human brain tissue allowed the researchers to study the development of the microglia over this time and monitor their response to changing environmental factors. Using in vivo two-photon microscopy, the team identified that the microglia actively surveyed their environment, responding to systemic indicators of inflammation and local injuries.
 Three advances in stem-cell-derived cardiac models and therapies
Three advances in stem-cell-derived cardiac models and therapies
We’ve collated recent cardiovascular disease research, including developing heart organoids with vascular cells and launching cardiac chips to the International Space Station.
Using fluorescence-activated cell sorting to isolate microglia from the organoids, followed by single-cell RNA sequencing, the team identified the protein SALL1 as being important in the conformation of microglial identity and the promotion of function. They also identified specific proteins that were required for the successful function of microglia.
Having conducted previous studies into the condition of macrocephalic autism spectrum disorder, the team had identified that the neurons of these patients grew rapidly and with more intricate connections when compared to neurons from neurotypical individuals. Curious to discover if these neuronal differences impacted microglial development, they decided to test the utility of their new platform.
The team compared microglia derived from individuals with macrocephalic autism spectrum disorder and those from neurotypical individuals with macrocephaly. They found that the neuronal differences previously observed persisted in this model and that due to this difference, microglia became far more responsive to injury or infection, illuminating a potential explanation for the increased inflammation often associated with the brains of individuals with autism spectrum disorder.
Though these results are interesting, the small sample sizes of only three individuals in each cohort mean that little can be conclusively inferred by this proof-of-concept study, a fact that the team would like to remedy with further, larger investigations.
Commenting on their future efforts to apply this method to other developmental and neurodegenerative diseases, first author Simon Schafer (Technical University of Munich, Germany) posited that, “by building our own brain model we can work from the bottom up and see solutions that may be impossible to see from the top down. We are eager to continue improving on our model and unraveling the relationship between the brain and immune system.”