Inspecting infection: how organoids helped map out sites vulnerable to SARS-CoV-2 infection
Refer a colleague
The response to the COVID-19 pandemic has involved action from a host of fields across the academic community. We have seen engineers working to rapidly produce effective ventilators, data scientists and epidemiologists collaborate to model the potential spread of the virus, economists predict the fiscal impact of the pandemics on society and molecular and cellular biologists work night and day in order to understand the nature of the disease and the mechanism of SARS-CoV-2 infection.
Within this last category, an array of techniques has been employed. One such technique, which has proven vital in establishing the tissues that can be infected and damaged by the virus, is the use of organoids as models for infection studies.
How can the gut be affected by COVID-19?
One of the first of these key studies was designed to explore the increasingly prevalent reports of patients with COVID-19 suffering from gastrointestinal issues in addition to the respiratory issues that first characterized the disease [1].
A research collaboration from The Netherlands, led by Mart Lamers (Erasmus Medical Center, Rotterdam, The Netherlands) and armed with the knowledge that the virus infects the epithelium of the lungs by interacting with the cell surface receptor ACE2, set out to explore the cause of these gastrointestinal symptoms.
Lamers and his team established 3D cell cultures that displayed the same spectrum of cells that compose the tissues of the small intestinal epithelium. These intestinal organoids were grown in a variety of conditions, leading to disparate numbers of ACE2 receptors in each organoid.
By exposing these organoids to SARS-CoV-2 and monitoring the subsequent progression of their infection using electron microscopy, the team was able to establish that the virus was capable of infecting the intestinal enterocytes of the organoids in both their progenitor and mature states.
The enterocyte cells – absorptive cells that form the epithelium of the small intestine – were found to produce infectious viral particles, indicating that the cells can be infected by SARS-CoV-2 and cannot prevent the virus from replicating. The rate at which each organoid was infected did not vary based on the proportion of ACE2 receptors present, suggesting that only a very small number of the receptors are required to enable infection.
What brain cells are infected by SARS-CoV-2?
As the pandemic continued and reports of further new symptoms did not abate, it became apparent that brain tissue needed to be assessed for its likely infection by SARS-CoV-2. Descriptions of headache, anosmia, confusion, seizure and encephalopathy accompanying the multitude of other symptoms of COVID-19 stimulated a research team from the Chinese Academy of Sciences (Shenzen, China) and the University of Hong Kong (HK) to investigate [2].
The team chose to investigate using an assortment of different cell models, including human neural progenitor cells (hNPCs), neurospheres and induced pluripotent stem cell-derived brain organoids.
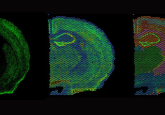
The brain organoids were grown to 35 days old, at which point the presence of fluid-filled ventricular-like structures – reminiscent of an early cerebral cortex – pan-neurons, early forebrain and hNPC markers were all detected.
The hNPCs were first evaluated to identify their content of ACE2 and other coronavirus entry-associated proteins. This exposed the presence of ACE2 and a sequence of other proteins capable of allowing coronaviruses to enter a cell, establishing that there was a clear mechanism by which these cells could be infected by SARS-CoV-2.
The hNPCs, the neurospheres and then the brain organoids were all challenged with SARS-CoV-2 and SARS-CoV as a control. The hNPCs were determined to be vulnerable to infection by SARS-CoV-2 but not SARS-CoV, while the neurospheres and the brain organoids displayed elevated protein expression and infectious viral particles, indicating that the virus was capable of infecting a human brain.
Further observations of the brain organoids revealed that the infection was restricted to TUJ1- (neuronal marker) and NESTIN- (NPC marker) positive cells. This indicates that cortical neurons and hNPC are at greatest risk of being infected and suggests that patients who have experienced neuronal symptoms of the disease should be monitored for long-term neurological effects of the disease.
Exploring how COVID-19 causes pneumonia
Organoid models of the lung in existence prior to the COVID-19 outbreak were quickly used by organizations to pivot their research and study the disease, leading to a lot of our initial understanding of the virus. However, many organoid models present a flawed representation of the lungs. This limits the depth of information that can be obtained from them, most notably the pathogenic mechanism by which SARS-CoV-2 leads to pneumonia and acute respiratory distress syndrome [3].
A key flaw in these models is a result of their inability to support the survival and growth of the stem cells that differentiate into secretory club (AT1) and alveolar cells (AT2), both responsible for repairing damaged lung tissue. Often, to include these cells, “feeder” cells are used to support their growth, impacting the composition of the organoid making it less representative and, therefore, less useful.
However, in a paper (yet to be peer reviewed) on bioRxiv, a research collaboration led by Stanford University (CA, USA) that included researchers from 10x Genomics (CA, USA) and the University of North Carolina at Chapel Hill (NC, USA) reports the successful establishment of organoids that contain self-renewing AT2 cells capable of transdifferentiation into AT1 cells. These organoids were referred to as AT2 Organoids.
They also established ‘basal organoids’ that formed ciliated lumens lined by differentiated club cells and contained two subsets of basal cells that contain the key mRNA markers of lung basal cells. The first set of basal cells showed indications of differentiation and proliferation, while the second displayed markers of vesicular and endoplasmic reticulum metabolism and squamous cell expression.
Already, these advances mean that the organoids provide a significantly more representative model of the human lung. However, not content with these improvements, the team looked to overcome another issue in lung organoids. Frequently, the basal cell portion of the organoid is directed towards the extracellular matrix – the medium through which the organoid would be exposed to SARS-CoV-2. Identifying this as a potential issue, blocking the ACE2 receptors that reside on the luminal surface of the lungs from interacting with the SARS-CoV-2, the team inverted their organoids with an eversion method, increasing the availability of the luminal ACE2 receptors to the SARS-CoV-2.
With their improved organoid models established, the team proceeded to infect the organoids with either influenza or SARS-CoV-2. They found that cells were easily infected by SARS-CoV-2 and that at 72-hours post infection the viral genome was being successfully replicated within the cells alongside the nucleocapsid protein. 10% of the cells in both the basal and AT2 cells were infected, with the majority of the infection in the basal organoids located in the AT1 cells.
This clearly shows AT1 and AT2 cells to be a novel target of SARS-CoV-2 and suggests that their disruption and subsequent loss of secretory properties could account, in part, for the pathogenesis of pneumonia.
From the very beginning of the pandemic, organoids have enabled researchers to model potentially vulnerable tissues and map out sites of infection that could be contributing to the nebulous list of symptoms associated with SARS-CoV-2 infection. These studies have identified many more than just the organs discussed in this article as being at risk of infection and damage, such as the heart, CNS and kidneys. But as organoids continue to evolve, driven forward by the pace of COVID-19 research, they provide much deeper insights into the nefarious workings of the disease and the mechanisms of action by which it inflicts its malicious wounds. With this information, comes the promise of new avenues to defend against the virus, and hope for a future that doesn’t involve accepting COVID-19 as “the new norm.”
Please enter your username and password below, if you are not yet a member of BioTechniques remember you can register for free.