First organoid model for neuromuscular condition reveals potential cure
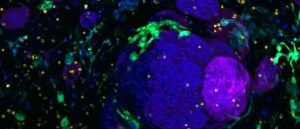
Scientists have developed the first human disease model for Fukuyama congenital muscular dystrophy using stem cells derived from a patient.
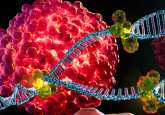
Fukuyama congenital muscular dystrophy (FCMD) is a neuromuscular disorder resulting from a mutation in the α-dystroglycan protein, which is responsible for muscle integrity. Fetuses suffering a lack of glycosylation as a result of this protein mutation develop severe muscular dystrophy, intellectual disability, seizures and insomnia. The life expectancy for those with FCMD is low, with patients seldom surviving into their 20s.
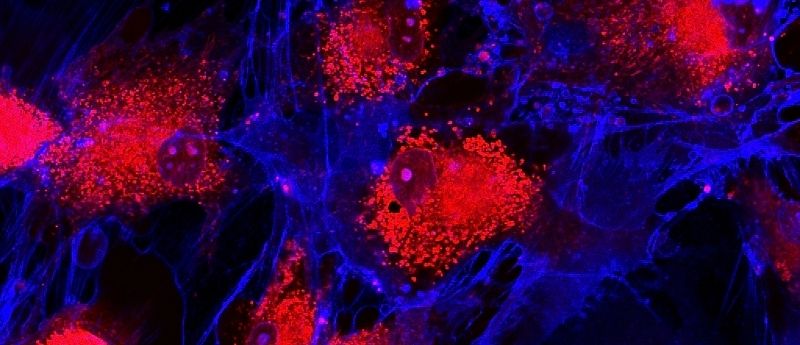
There is currently no known cure for FCMD, however, scientists from Japan and the USA, led by Mariko Taniguchi-Ikeda (Fujita Health University Hospital, Aichi, Japan), have recently developed the first human model for the disease, utilizing stem cells from an FCMD patient. The team was able to transform the patient-derived pluripotent stem cells into skeletal muscle and brain organoids. Their study outlines the capabilities of a small compound, Mannan-007 (Mn007), to reduce the defects associated with this model.
Improving organoid mimicry and reproducibility
A new synthetic gel enables the generation of representative, reliable pancreatic organoid models of healthy and cancerous tissue and many other tissue types.
Taniguchi views the search for a cure as a lifelong pursuit, with more than 20 years in the field thus far, stating that, “I understood the importance of attempting to cure this disease. But first, we needed a better model to study FCMD in the laboratory.”
Using the brain organoid model, researchers illustrated restoration in the ‘radial architecture of neurons and cortical plate organization’. By successfully mimicking FCMD, the brain organoids revealed neuronal migratory impairment as a result of disarray in the radial glia. As animal models do not completely reproduce these anomalies, the human disease model is proving superior.
“We hypothesized that the addition of a molecule like Mn007 that can promote αDG glycosylation would rescue the defects observed in FCMD.” Dr Taniguchi-Ikeda explained. Their hypothesis proved valid: when tested, Mn007 demonstrated an ability to restore αDG levels in both the muscle and brain models.
Their research, published in the journal iScience, emphasizes the importance of αDG glycosylation, highlighting the opportunity to explore migration defects related to a lack of αDG glycosylation. While a cure for FCMD is still a long way off, the study draws attention to the potential of molecules likeMn007 to be utilized in treatments for FCMD and similar diseases.