Will the COVID-19 pandemic help end systemic racism?
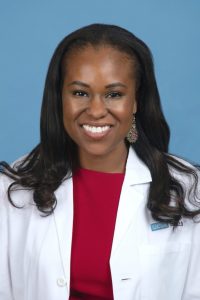 Dr Fola May has focused her career on health inequity research. Now, the coinciding COVID-19 pandemic and Black Lives Matter protests have highlighted pre-existing racial disparities and thrown her research into the spotlight.
Dr Fola May has focused her career on health inequity research. Now, the coinciding COVID-19 pandemic and Black Lives Matter protests have highlighted pre-existing racial disparities and thrown her research into the spotlight.
What impact has the COVID-19 pandemic had on your research?
Our team at UCLA focuses on cancer and healthcare disparities. Specifically, we look at how we can improve cancer outcomes for people who are marginalized or medically underserved. Before COVID-19, we were deeply engaged in our research to impact underserved communities, trying to improve the number of Blacks and Hispanics who get screened for cancer, and trying to decrease mortality from cancers in Blacks, Latinos and other marginalized groups.
Then COVID-19 hit. It was devastating to our current projects because we couldn’t reach out to recruit for our studies. The focus in many of the clinical settings in which we work became curbing the virus. That was understandable, but we worried about losing ground in so many other critical health conditions. For example, there was an 86% reduction in colon cancer screening in the USA in the month of March. This is a cancer that is largely preventable and for which screening is already suboptimal, and, in a fell swoop screening for it came to a standstill.
We are still very concerned about the number of cancers and the deaths from cancers that will result from the interruption of preventive services during COVID, so a lot of our work right now is focusing on the impact of COVID on cancer prevention and care.
Can you summarize the findings of your recent review in Nature?
The piece highlights that while coronavirus is a horrible pandemic, it is one of two pandemics that we are fighting right now. COVID-19 is shedding light on a decades-long pandemic of systemic racism in the world – those inequities are manifested as health disparities and are caused by social determinants of health. Social determinants of health are the conditions in which individuals live and work and the exposures that an individual has as a result of those conditions that contribute to their health outcomes.
I always like to say where you are born largely predicts your health. If, for example, you are born into poverty in an environment where there is no access to healthy foods, safe spaces or education, you are more likely to have an unhealthy diet, exposure to violence, and other influences that lead to poor health outcomes like diabetes, hypertension, and premature death. Those living environments are the predisposing factors that make vulnerable populations at baseline very different from advantaged populations.
When COVID-19 hit, it hit these populations disproportionately. Everyone wanted to focus very early on the fact that COVID-19 was killing Blacks and said, well COVID-19 is killing Blacks because Blacks have more diabetes and more obesity and more heart and lung disease. Those things are true but what we wanted to highlight in this piece is that we actually have to take a step back and realize that it’s not just the diabetes and asthma, it’s the environment in which Blacks live in the USA that’s led to these health conditions that have made them vulnerable to COVID-19. And, unfortunately, unfair and unjust policies and racism have led to these environments.
What are the necessary steps to improve these disparities?
My co-authors and I felt it was going to be very important to not only explain social determinants of health as the root of the problem but to also provide solutions. Fixing the disparities is about fixing the upstream social determinants of health, which, in turn, can impact many health outcomes. So, we outlined three major recommendations.
The first is that there needs to be support at the federal level, the state level and the local level for health disparities research. We need additional funds allocated to understand why differences in care and outcomes occur and to address the inequities that exist. We also need funds to increase diversity in the healthcare workforce because if we don’t have Black, Hispanic and Native American doctors and nurses, we are unlikely to have people who champion these problems.
The second recommendation is that we need to be honest that racism is real. A lot of people want to put a veil over racism or say it doesn’t exist, but as a nation we need to declare it a crisis and promise to make it go away. That will require insight and support from the government, national legislative priority and working towards dismantling the discriminatory practices that are in place in the USA.
The third thing is that vulnerable populations – Blacks, Hispanics and Latin Americans – need to be participating in change. They need to be given a voice. If we are to come up with effective solutions in the USA, we need to partner with organizations and communities to make sure that they have a hand and a role in creating the solutions so that there is lasting impact.
There have been some discrepancies with how the USA has been assigning COVID-19 deaths, has this been an issue in your research?
One of the biggest problems recognized early during COVID-19 was that in the USA, we don’t capture good data on race and ethnicity. For us to understand who is dying from the disease, we need reliable data on who is getting the disease and that involves information about their racial background and their ethnicity. Unfortunately, in many hospitals that is not reliably captured.
We knew, for example, that 1000 people had died in one city, but we had information on racial background for only 20% of them. Now there is more attention towards getting better data, having the infrastructure and funding in place, and mandating that hospitals report race and ethnicity in the USA. It’s still not perfect, and I think that is why assigning deaths to a certain race and ethnicity has been challenging.
The other thing that has been an issue is attributing deaths to COVID-19. For example, a hospitalized individual may die from a pneumonia that’s not related to COVID-19 or have a heart attack at the same time they have COVID-19 infection. In these cases, do you consider COVID-19 the cause of the death? So, in some cases it has been challenging to define the cause of death and to determine whether it was attributed to COVID-19.
The WHO and the CDC have since created definitions for how to ascribe a death to COVID-19, which has been helpful, and a lot of institutions have adopted those.
 Why are Black people more likely to die of COVID-19 in the US and UK?
Why are Black people more likely to die of COVID-19 in the US and UK?
Just as the current protests in the USA highlight racial inequalities in the US justice system, COVID-19 is directing a spotlight at inequalities and systemic racism in healthcare and medicine.
If it weren’t for the pandemic and the Black Lives Matter movement highlighting pre-existing racial disparities, do you think we would be in a different position now?
I do. The reality is that researchers have been doing work in health disparities for decades, and it just wasn’t getting the recognition it deserved. COVID-19 is shining a bright light on a problem that we have had for a long time. Despite all the horrible things that have come with COVID-19, it has given us the opportunity to bring this problem to the surface so that it is finally receiving the attention it deserves.
What are the challenges of being a Black physician and scientist?
There are very few of us; Black women make up 2% of doctors in the USA [13.4% of Americans are Black]. When you are part of a group that small, you are constantly facing aggressions and micro-aggressions. There are patients who don’t want us to touch them or people who automatically assume we are not physicians despite the fact that we are wearing a white coat with the word doctor in front of our name. I have been in multiple scenarios where I have had to smile and move on despite unjust treatment by patients and family members. White patients— and only White patients— often ask me where I went to medical school immediately upon meeting me— it’s a passively aggressive attempt to question my credentials. When you are dealing with those aggressions daily it is exhausting. It’s a heavy burden to carry in addition to all the usual stressors of providing care for ill people.
Despite that, Black doctors and scientists are working hard to carve out a role for ourselves in academia. We are less likely to be promoted in the academic setting and we are less likely to be in positions of leadership as deans, division chairs, directors and department heads. We also have to deal with colleagues who unfortunately don’t think that we deserve to be where we are. We are constantly defending ourselves and know that we need to be twice as productive as our non-Black colleagues sometimes to gain recognition.
I worry that there is no focus on cultivating and mentoring Black academics. Many Blacks leave academics out of frustration and feeling undervalued. We need to do a much better job of identifying people who are going to be successful in science, bringing them into the workforce and doing everything that we can to make sure that they stay in the workforce, which means mentoring them, promoting them and giving them leadership roles. Currently, we are not doing that.
Do you think that there is more that individual institutions and white colleagues could be doing?
Absolutely. I think there is a lot more that our colleagues can be doing. And I don’t think that the problem is that they didn’t want to do anything. The problem is that because they are not Black, they were not readily seeing what is happening. They are surprised upon realizing that they can count on one hand the number of Blacks in their division or department. They are shocked to hear the stories of blatant racism. Now, we are trying to put this all out in the forefront so that they have to recognize this is happening. We are also telling our academic colleagues that we must act, and we must do something to make this situation better.
We must increase the pipeline for Black scientists, starting earlier to get Black youth into science. We must improve mentorship and make better mentor programs so that Blacks are retained in science. We must increase the number of Blacks in leadership roles. And we should increase funding and resources for health disparities research.
Find out more – read “From words to actions to change: How medicine, academia can respond to racial injustice.”
Are there any factors that are more prevalent in the racial disparities for cancer patients, or is there a combination of factors?
It’s a combination of factors. There are provider factors, patient factors and factors related to the healthcare system. Let’s start with the patient factors. Sometimes patients don’t know that screening is recommended. There is also a lot of hesitancy to trust the medical profession. Given that Blacks in the USA were experimented on in medical hospitals for decades and now knowingly often receive worse quality care than Whites, how can you blame them for the lack of trust?
Concerning provider factors, sometimes providers unfortunately discriminate against patients. Sometimes it’s knowingly and other times it is subconscious. I think most often I see doctors who delay recommending a treatment to a minority patient who they don’t see as benefiting from the treatment or wanting the treatment. Little changes in the recommendations doctors make can impact how well a patient fares with a disease.
The system level factors impact low income Americans most, which happens to be Blacks and Latinos. Lack of healthcare insurance and variable quality across health centers impact health outcomes. Because we don’t have a universal health system where everyone has insurance, many individuals are disadvantaged even before they become ill. We certainly are in need of healthcare reform that promotes better health for all in our nation.
If you would like to keep up to date with our content on coronavirus, you can sign up for our site here, where you can subscribe to our newsletters for free!