Researchers use CRISPR gene editing to uncover potential HIV treatments
Using CRISPR researchers have identified 86 genes that could be associated with HIV replication and disease, opening doors to research on how the virus behaves in the body.
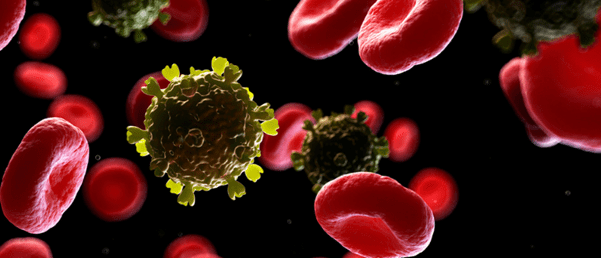
A research team from Northwestern Medicine (IL, USA) has published the results of a study utilizing advances in CRISPR gene editing technology to identify potential treatments for HIV. The team aimed to understand how HIV establishes infection in the human body and how the virus uses cells to spread across the whole physiological system. To do so, the team utilized CRISPR to deduce the human genes necessary for HIV to infect the blood.
During the study, T-cells – the major cell type that is targeted by HIV – were isolated from donated human blood and hundreds of genes were knocked out with CRISPR-Cas9. The knock-out cells were then infected with HIV and analyzed by the team.

Novel stem-cell transplants could be an HIV cure
The first female, nonwhite and HIV-positive cancer patient treated with a new stem-cell transplant therapy is now in long-term remission suggesting a potential HIV cure.
One of the knockouts was a gene involved with viral replication, which resulted in a decreased rate of infection. In addition, cells that lost an antiviral factor exhibited an increase in infection rate. The research team then confirmed the identified factors by selectively knocking them out in further donors, finding a series of novel and known pathways.
Researchers discovered 86 genes that might be involved in HIV’s replication and pathogenesis, including over 40 that have never been looked at in the context of HIV infection. In addition, the study proposes a new map that can be used to understand how HIV integrates into DNA and establishes chronic infection.
In previous studies, researchers have relied upon the use of immortalized human cancer cells as models to study how HIV replicates. These kinds of cells are easily manipulated in the lab but they are imperfect models of human blood cells.
Also, most of these studies utilize technology to turn down the expression of certain genes, but not turn them off entirely, meaning that researchers cannot always determine if a gene was involved in aiding or suppressing viral replication.
Judd Hultquist, co-corresponding author of the study, stated: “with the CRISPR system, there’s no intermediary – the gene is on or off. This capability to turn genes on and off in cells isolated directly from human blood is a game changer; this new assay is the most faithful representation of what’s happening in the body during HIV infection that we could easily study in the lab.”
The researchers hope to continue and aim to develop a technology that will enable genome-wide screening to locate all potential HIV host factors. This would represent another step towards uncovering longer-term treatments for the virus.