Nanoparticle sensors differentiate bacterial and viral pneumonia
Researchers have developed a nanoparticle sensor that can distinguish bacterial pneumonia from viral pneumonia, which could be used to determine the appropriate course of treatment.
Senior author Sangeeta Bhatia and colleagues from the Massachusetts Institute of Technology (MIT; MA, USA) have developed a sensor that can indicate the microbial cause of pneumonia infections in just two hours. This could be an important diagnostic tool for doctors when deciding the proper course of treatment as improper prescription of antibiotics could lead to antibiotic resistance, a growing problem for public health.
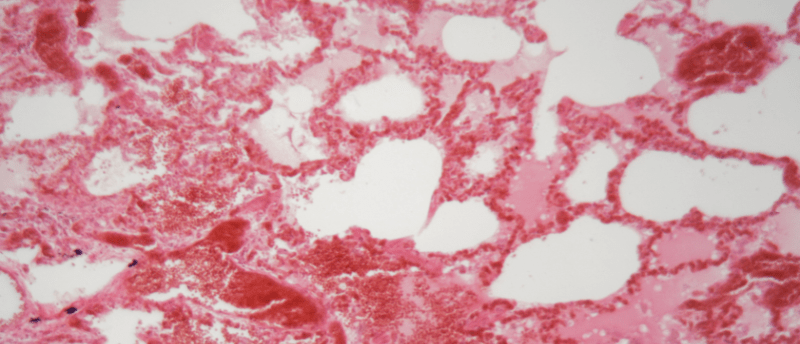
Pneumonia is an infection of the lungs, which can be caused by viruses (influenza and respiratory syncytial virus) or bacteria (Streptococcus pneumoniae and Haemophilus influenzae). Due to the many microbes that can cause pneumonia, it can be difficult to identify the exact cause and select the appropriate course of treatment. To address this issue, Bhatia’s latest study set out to design a diagnostic tool that could recognize the different immune responses generated depending on whether the infection is viral or bacterial.
 Boosting fluorescent sensors to get a WIFF of successful glioblastoma treatment
Boosting fluorescent sensors to get a WIFF of successful glioblastoma treatment
Researchers from MIT developed a novel photonic technique to enhance the signal emitted by fluorescing nanosensors, improving the signal-to-noise ratio by 50-fold and allowing for deep tissue detection.
To establish a readout for immune responses to different pneumonia infections, the researchers mined 33 datasets of genes expressed in response to respiratory infection, which enabled them to identify 39 proteases that respond differently depending on the type of infection. Proteases are released by immune cells in response to specific infections, in order to degrade key proteins present in a pathogen.
With these 39 proteases established, the research team designed 20 nanoparticle sensors that can recognize different proteases. The sensors are peptide-covered nanoparticles that are cleaved by a specific protease, releasing a reporter molecule that eventually makes its way into the urine. An analysis of a urine sample using mass spectrometry indicates which proteases are active in the lungs.
Using five mouse models of pneumonia caused by three different bacteria and two viruses, researchers injected the sensors into the trachea to test these sensors against known infections. Machine learning allowed them to automate the differentiation process, distinguishing healthy cells from infected ones as well as the pathogen responsible for infection. The sensor was demonstrated to differentiate between viral and bacterial infections and could even tell the difference between the five pathogen models tested, albeit with lower accuracy.
Researchers are continuing to advance the sensors to be applicable to human diagnostics, which must account for greater genetic variability. For human administration, an inhaler is being developed to deliver sensors to the lungs. Additionally, by utilizing urine tests the sensor could be adapted as a quick and easy diagnostic resource at home. The potential to decipher the type of pathogen responsible for pneumonia and create a simple urine test provides hope for an effective tool for the diagnosis and treatment of pneumonia.