Key tips and technologies for the development of iPSC-derived cell therapies
Nicola Bevan is a manager in the BioAnalytics Applications Group (Royston, UK) of Sartorius (Göttingen, Germany). Her team is focused on the development of novel applications and delivering customer-facing data to showcase their range of bioanalytical instruments and their applications in different fields of biological research.
Here, Nicola discusses the field of iPSC-derived cell therapies, highlighting significant challenges and how these can be addressed through the integration of Sartorius’ instruments into cell therapy development workflows.
Please could you give a brief overview of the cell therapy development pipeline?
Process development for induced pluripotent stem cells (iPSCs) requires multiple steps. First, you need to isolate your primary cell of choice before expansion. Next, these cells need to be reprogrammed to induce pluripotency before you then select the best clones to proceed with. Gene editing may be required at this stage to imbue the cells with specific histocompatibility profiles.
With these processes complete, further clone selection and expansion steps take place to produce a master cell bank and working cell bank. During these stages, pluripotency is continually assessed to ensure the cells maintain this property.
With your working cell bank established, you then induce differentiation to produce the cell lineage of interest for your therapy. This is often a lengthy process that involves multiple technical steps and checks to ensure that the correct phenotype and function have been instilled in the final differentiated cells.
Finally, the system needs to be scaled up to enable the production of the significant amount of cell product required for clinical use. All the while, the sterility and functionality of the product are assessed to ensure that it is suitable for clinical use.
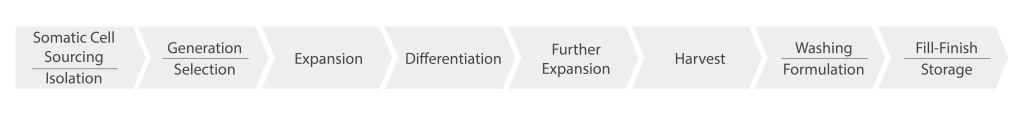
Figure 1: A schematic of the steps involved in the development of iPSCs for cell and gene therapies.
What are the advantages of using iPSCs as the starting cells in this pipeline over other cell types?
Pluripotent stem cells, including iPSCs and embryonic stem cells (ESCs), have the innate ability to self-renew indefinitely and differentiate into many cell types. This confers a unique advantage when compared to other cell therapies, such as adult stem cells, cancer stem cells, or somatic cells, since the starting cells can be differentiated into any specific cell type required for the final therapy and have the capacity for infinite expansion.
The ability of iPSCs to self-renew means they could replace the use of ESCs and overcome various associated ethical issues. iPSCs, like ESCs, are amenable to genetic modification prior to differentiation, which enhances the impact of the targeted therapeutic by yielding not only the desired phenotypic characteristics but also the genetic characteristics required to maximize efficacy. By using patient-derived iPSCs, it is also possible to eliminate or reduce the chance of the cell therapy being rejected by the host immune system.
Furthermore, iPSCs enable the development of specific, physiologically-relevant cell and tissue models, such as organoids, which have increased translational value compared to traditional 2D cell cultures. These models can be useful in assays to determine the efficacy of novel iPSC-derived cell and gene therapies, for example, in the neuro space, where sourcing primary human tissue is challenging. Furthermore, the use of patient-derived iPSCs to establish these models enables the testing of specific treatment regimens to determine which would be optimal for a patient, personalizing their therapy.
What are the biggest obstacles when it comes to developing iPSCs?
iPSCs are high maintenance, expensive and require constant monitoring to ensure they maintain pluripotency, viability and homogeneity. Long-term culture of iPSCs can result in genotypic and phenotypic heterogeneity, even in a cell line derived from a single source cell. Therefore, it is vital that methods for monitoring, detecting, and reducing heterogeneity in iPSC lines are developed.
The increasing use of stem cells in clinical and research settings calls for fast, robust and cost-effective solutions for the growth, characterization and maintenance of these valuable biological resources.
Do you have any tips for best practices to ensure successful process development for iPSC-derived cell therapies?
Certainly! There are several key things to consider. You need to establish tight control of the whole process, ensuring that meaningful screening is conducted throughout, sufficiently optimizing each step to efficiently produce a homogenous and sterile product and to deliver a product and production line that is scalable.
One of the key ways this can be achieved is by automating as many of the processes as possible to reduce operator-to-operator variability and facilitate a higher throughput. You need screening systems that can keep up with this throughput to enable rapid process optimization, which is a big factor in the scale-up side of things. As mentioned earlier, you need to continuously characterize iPSCs and derivatives throughout the differentiation process to ensure the cell type and quality of the resulting cells to deliver that high-quality, effective product.
Finally, you need detailed insight into the performance of your process by setting and monitoring critical process parameters (CPPs) and critical quality attributes (CQAs) to measure the success of your process and enable seamless scale-up.
What technologies does Sartorius offer to address those challenges?
Our portfolio of solutions for iPSC therapy is designed to help identify differentiation protocols to generate target cell and tissue types, accelerate process development, and implement consistent, high-quality manufacturing.
Sartorius offers a range of research-use only (RUO) and GMP growth factors and cytokines for the expansion and differentiation of iPSCs. These are of high purity, stability and reproducibility and ensure a seamless transition from R&D stages to pre-clinical development and commercial manufacturing in a GMP environment.
In the research and development stages, the Incucyte® and iQue® platforms offer unique, high-capacity solutions for characterizing cell phenotype and function at unprecedented speed, depth, and scale. They enable easy tracking of changing phenotypes during differentiation and rapid sampling with low volume requirements, walk-away imaging for growth tracking and analysis, and high-throughput screening capabilities.
Additionally, CellCelector offers the ability to select iPSC clones or areas of clones of interest for further expansion in a fast and gentle fashion. This early-stage development with rapid screening and optimization of differentiation processes can then be linked to a clean transition to manufacturing.
One of the key challenges in the development of cell therapy products is the need to ensure sterile conditions throughout the entire process. Any contamination can lead to serious health risks for patients, therefore it is critical to have reliable methods for testing the sterility of these products at several stages of the process and prior to administration. The Microsart® ATMP Sterile Release Kit is specifically designed to meet this need, offering a fast and accurate way to test the sterility of ATMPs and other short shelf-life products.
If there was one tool or insight that you could wish for to help improve the development of iPSCs for use in stem cell therapies, what would it be?
I would wish for an increase in the amount of the process that can be automated to reduce the risk of cell infections and minimize hands-on time in the lab. I would also really like a technique that could provide image-based identification of the best time to passage or differentiate cells.
This interview was produced in association with Sartorius.