Genetic ancestry: one piece of the immune response puzzle

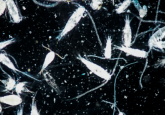
The differences in early immune response to influenza viral infection are shaped by genetic ancestry in a cell-type specific manner.
Researchers from the University of Chicago (IL, USA) and University of Minnesota (MN, USA) investigated the immunological differences in susceptibility to viral infection according to genetic ancestry. Led by Haley Randolph (University of Chicago), the study utilized single-cell RNA sequencing (scRNA-seq) of immune cells infected with influenza A virus to uncover the infection induced gene signatures. The group found that these different signatures occurred in a cell-type-specific manner linked with genetic ancestry.
The study aimed to uncover how individuals from diverse populations respond differently to infectious disease. In contrast to the COVID-19 pandemic we see today, before the advent of modern travel and globalization, viral infection cases were geographically contained to the area of the outbreak. Due to the strong selection pressure that viruses pose in the history of human evolution, these past viral epidemics may have driven population divergences in the immune response.
Randolph’s team took peripheral blood mononuclear cells (PBMCs) from males of different degrees of European- and African-ancestry and infected these with influenza A virus using in vitro infection assays. PBMCs are a group of specialized immune cells that are activated in the innate immune response to infection. Using scRNA-seq, the authors demonstrated that different immune pathway components in different immune cell types were activated in response to the influenza infection.
 Paleovirology paves the way: hepatitis B virus evolution mapped out
Paleovirology paves the way: hepatitis B virus evolution mapped out
Researchers collate hepatitis B virus (HBV) genomic data over the past 10 millennia using DNA-enrichment techniques to reconstruct large proportions of ancient HBV genomes.
“In contrast to bulk (traditional) RNA-seq, scRNA-seq allows us to evaluate how individual cells are transcriptionally altered in response to the virus without having to sort the cells, therefore preserving the critical interactions observed in vivo between the many different cell types involved in an efficient immune response to influenza A,” explained senior author Luis Barreiro (University of Chicago), speaking to Genetic Engineering & Biotechnology News (GEN).
The gene expression levels that were altered in response to influenza infection varied significantly depending on the individual’s ancestry. “We found that individuals with a higher proportion of European ancestry showed an increase in type I interferon pathway activity during early influenza infection,” said Barreiro, speaking to GEN. Interestingly, the genetic ancestry effects are highly cell-type specific, however the results do not indicate genetic differences in disease susceptibility – genetics may have a role, but it is not the only factor.
“Our findings suggest immune response variation may interact with or exacerbate environment-driven health disparities in viral susceptibility and morbidity, which occur for both influenza and COVID-19,” Barreiro clarified to GEN. “A lot of what we’re capturing could be the result of other disparities in our society, such as systemic racism and healthcare inequities.”
The team plan to expand their future research into factors affecting differences in interferon and immune response signaling in response to other viruses, such as SARS-CoV-2, and in a wider array of ancestry groups.