Newly discovered pathway provides potential key to prevent adverse effects of immunotherapy
Researchers identify a possible therapeutic target to prevent endocrine autoimmune adverse effects during checkpoint inhibitor immunotherapy.
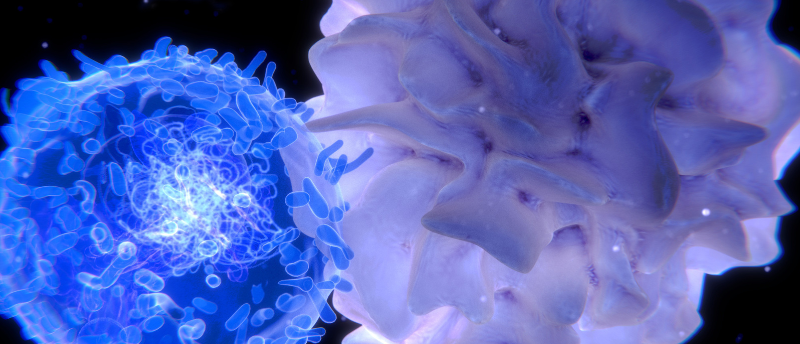
A study led by researchers at the University of California, Los Angeles (CA, USA) has revealed that interleukin-21 (IL-21) plays a role in the autoimmune attack that can occur following checkpoint-inhibitor cancer therapy, finding it controls the activity of CD8+ T cells. The researchers suggest that this pathway could be a potential therapeutic target to reduce endocrine autoimmune side effects.
Checkpoint inhibitors are a type of immunotherapy that block checkpoint proteins on the surface of T cells, preventing them from being turned ‘off’ in the tumour microenvironment and allowing them to kill cancer cells. This has proven to be successful in treating different types of advanced cancers; however, the increased immune activation can result in an autoimmune attack on healthy tissues, causing complications in up to 60% of patients treated with checkpoint inhibitors.
This autoimmune toxicity can result in organ damage and a lifelong requirement for hormone replacement therapy. The cause is largely unknown and there are no effective treatments currently available.
To understand the cause of immunotherapy-related autoimmune adverse effects, the researchers of this study focussed on immune checkpoint inhibitor thyroiditis (ICI-thyroiditis), an immune-related adverse effect that can result in the destruction of thyroid tissue.
 The future of lipid nanoparticles and mRNA cancer vaccines
The future of lipid nanoparticles and mRNA cancer vaccines
mRNA vaccines would not have been possible without breakthroughs in lipid nanoparticles, both of which researchers are now developing for cancer therapeutics.
Using single-cell RNA sequencing, the researchers compared immune infiltrates present in thyroid specimens from individuals with ICI-thyroiditis to samples from those with spontaneous autoimmune Hashimoto’s thyroiditis and those with no thyroid disease. This revealed increased amounts of clonally expanded effector CD8+ T cells that express CXCR6+ Granzyme B+ and interferon gamma+ in samples from those with ICI-thyroiditis, but not in the other sample types. This is a group of immune cells with strong cell-killing activity.
The study also found that IL-21 from CD4+ T helper cells, a soluble molecule that has regulatory effects on cells of the immune system, drives the thyrotoxic function of CD8+ T cells. These results were validated in vivo by inhibiting IL-21 in a mouse model. This inhibition prevented checkpoint inhibitor-associated thyroid autoimmunity, indicating that IL-21 could be a possible therapeutic target to reduce endocrine autoimmune side effects.
“Our study is the first to provide an in-depth look at the cause of checkpoint inhibitor-associated autoimmunity in humans and highlights a potential pathway for preventing this treatment-related autoimmune toxicity,” said Melissa Lechner, the first author of the study.
These results could lead to a strategy to make checkpoint inhibitor immunotherapy treatments safer and reduce endocrine autoimmune side effects. Additionally, this mechanism could be shared with some spontaneous immune diseases, like type 1 diabetes, meaning these findings could also lead to new therapeutic targets for a range of autoimmune diseases.