Boosting fluorescent sensors to get a WIFF of successful glioblastoma treatment
Researchers enhance the signal emitted by fluorescing nanosensors, improving the signal-to-noise ratio by 50-fold, allowing for deep tissue detection.
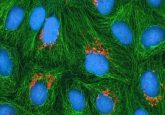
Fluorescent sensors can be used to label and image a variety of molecules in living cells; however, the fluorescent signal is lost if the sensors are implanted too deep into tissues. To overcome this, researchers from the Massachusetts Institute of Technology (MIT; MA, USA) have developed a novel photonic technique (a technique using light waves) for exciting any fluorescent sensor, thereby improving the resulting signal.
Quantum dots (semiconducting nanoparticles that are luminescent), carbon nanotubes and fluorescent proteins can be used to label molecules inside cells, and a fluorescent signal is triggered by shining a laser light. However, this is only possible in cells grown in lab dishes or tissues close to the surface of the body, otherwise the sensor’s fluorescent signal is lost to autofluorescence – the intrinsic fluorescence emitted from living tissues. “All tissues autofluoresce and this becomes a limiting factor,” explains Volodymyr Koman, one of the lead authors of the study. “As the signal from the sensor becomes weaker and weaker, it becomes overtaken by the tissue autofluorescence.”
So, the researchers developed a technique they call ‘wavelength-induced frequency filtering’ (WIFF) in order to enhance the fluorescence from the sensor so it can be differentiated from autofluorescence. WIFF modulates the frequency of the emitted fluorescence and is made up of three lasers to produce a laser beam with an oscillating wavelength. The researchers hope to use a tuneable laser to improve the technique further in the future.
“The technique works at any wavelength, and it can be used for any fluorescent sensor,” says Michael Strano, who leads the research group. “Because you have so much more signal now, you can implant a sensor at depths into tissues that were not possible before.”
 Laser-accelerated proton therapy: quickening the pulse of cancer treatment?
Laser-accelerated proton therapy: quickening the pulse of cancer treatment?
Researchers in Germany have, true to form, created an incredibly efficient laser, which they have tested on animals for the first time, marking a proton irradiation milestone in the process.
The researchers report that by shining this oscillating beam on the sensor, the frequency of the resulting fluorescence doubles. This means it can be more easily distinguished from the background autofluorescence and enhances the signal-to-noise ratio by more than 50-fold, hence it can be implanted deeper into tissues.
“If you have a fluorescent sensor that can probe biochemical information in cell culture, or in thin tissue layers, this technology allows you to translate all of those fluorescent dyes and probes into thick tissue,” says Koman. In this study, the researchers showed that fluorescent sensors could be implanted at 5.5cm in the tissue, whilst still obtaining a strong signal.
WIFF could mean that these fluorescent sensors can track molecules in deep tissues to monitor the effect of drugs or be used as a diagnostic tool. The researchers used WIFF to monitor chemotherapeutic drugs in treating glioblastoma, a form of brain cancer. In glioblastoma, the tumor is first surgically removed followed by chemotherapy using temozolomide (TMZ) to kill any remaining cancer cells. However, TMZ has severe side effects and is not effective for all patients, therefore being able to monitor the drug would be beneficial.
TMZ gets broken down into several smaller compounds including AIC, so the research team designed a fluorescent sensor to detect AIC and used WIFF to improve the signal-to-noise ratio. They showed that sensors could be implanted at 5.5cm within an animal brain, and the signal could still be detected even through the skull.
The researchers also showed that WIFF could enhance the signal from many sensors including carbon-nanotube-based sensors that Strano’s lab previously designed to detect hydrogen peroxide, riboflavin and ascorbic acid. Similar sensors could be developed to detect oxygen species or other molecular signals of tumor cell death.
“We are working on technology to make small sensors that could be implanted near the tumor itself, which can give an indication of how much drug is arriving at the tumor and whether it’s being metabolized. You could place a sensor near the tumor and verify from outside the body the efficacy of the drug in the actual tumor environment,” says Strano.
The researchers are now developing sensors that are biologically resorbable, to avoid surgical removal of fluorescent sensors.