Child’s play: how a children’s toy inspired a wearable respiration sensor
A wearable respiration sensor, with the potential for continuous monitoring straight to a cell phone, has been developed from a popular children’s toy, Shrinky Dinks. Michelle Khine and Michael Chu explain.
Michelle Khine
Michelle was an assistant and founding professor of the School of Engineering at UC Merced. Prior to that, she received her BS and MS in mechanical engineering from UC Berkeley and her PhD in bioengineering from UC Berkeley and UCSF (all CA, USA). She co-founded Fluxion Biosciences (CA, USA), Novoheart (BC, Canada) and TinyKicks (CA, USA), and is currently based at UC Irvine (CA, USA), where she has been for the past 10 years.

Michael Chu
Michael grew up in the Silicon Valley surrounded by a lot of technology. He received a BS in bioengineering from UC San Diego (CA, USA) before applying to graduate school, ending up in Michelle’s lab, where he’s been for the past 5 years.
“I fell into wearable technology serendipitously because I entered Michelle’s lab right when we started this area and I’ve watched it grow since then, which is really neat.”

What are Shrinky dinks, and how did the idea first come about to utilize them in a laboratory setting?
Michelle started off as the assistant and founding professor at a new University of California site, but this was in Merced, which is out of the way of any big cities, and because they were very new, they did not have any of the machines and technology needed to do microfabrication. A lot of what we do in microfabrication is very small, even dust particles can interfere with the manufacturing, and so it became very difficult for her to work.
She started thinking if there was anything else she could use for her work, and then she got inspiration from one of her favorite childhood toys, the Shrinky Dink. Shrinky Dinks are pieces of plastic that kids draw on and when put into an oven, they shrink to a much smaller size. Michelle wanted to see if she could make these microfabricated devices using Shrinky Dinks in the oven; it worked and that’s how she first started using it in the lab.
When she first started, and she came out with this idea, her students weren’t sure if it was going to work – “you want to what?! With a children’s toy?” etc. – but it actually worked really well and that’s what’s brought us to where we are today.
How were the Shrinky Dinks utilized in developing the sensor?
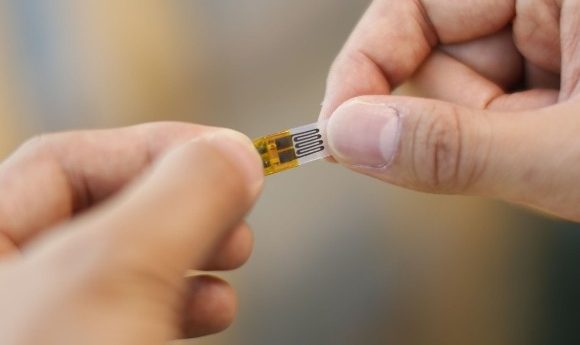
We use the Shrinky Dink as a platform for flexible electronics. They do two things; the first is that we can create our sensor at a very large size and then we can shrink it down so it’s smaller. It gives us the ability to create a very detailed sensor without needing the actual equipment to do so.
The other thing is that when you shrink metal on them, they allow the metal to be more flexible. Using this we were able to create these very sensitive strain sensors. So we took this technology and started applying it to the body to see what type of information we could get out of it.
One of the first things we wanted to look at was respiration, particularly respiration volume and respiration rate. We placed these strain sensors on two locations on the abdomen and used it to track the movement of these two locations. Using the data gathered from these two locations, you can calculate the respiration volume and the respiration rate, which is not something that a lot of wearable sensors do.
What are the sensor’s advantages in comparison to standard sensors?
The medical standard is a medical grade spirometer, which are devices that you breathe in to and out of. They aren’t portable and you have to use them in a doctor’s office, which means they don’t offer continuous monitoring of your health. This makes it difficult to identify any disease or condition that worsens over time.
The advantages of these sensors are that hopefully in the future they’ll be portable. We can track the patient continuously over time and catch any symptoms that come forth and address them immediately. There are other technologies that can track respiration wirelessly, but these tend to be very bulky. Our sensors are about that of a band aid, so when you put it on, the hope is that the patient will forget that they’re wearing it and just be able to go about their daily life.

What were the results when the sensor was tested?
On the initial testing, we had a couple of subjects all laying down; we placed the sensor on the stomach and the ribcage, and we took measurements concurrently with the medical grade spirometer.
There was a really good agreement between our calculated respiration volume and the volume that we measured using the continuous spirometer. We could also track rate as well. Those are the two things that doctors look at for respiration, as well as flow, which is something we’re looking into right now. We have some preliminary evidence that shows that we can also calculate respiration flow, but we need to do a little more research into that.
What are the other next steps for the technology?
There’s a lot; there’s always a lot in research. One of the things we need to do to make sure these sensors work in the real-life environment is to ensure that we can still get a good signal while the subject is outside walking or running. So, we’re looking at what kind of motion artefact we get in the sensor as someone’s walking, running, or biking.
In the future, we want to apply artificial intelligence to it. We’ve developed a sensor that can gather a lot of data; so much data that a person can’t realistically go through it in a day to look for any problems. So, we want to apply artificial intelligence to analyze the data continuously so it can pick up any disturbances in breathing and alert the subject, or the subject’s parents, or the care giver. That’s the next step in any kind of wearable technology; to start using machines to analyze our health and be able to alert us when something is going wrong.
We’re also in the process of commercializing the sensor, too. We’re looking to take this out of the lab and into the commercial market, or into the medical market.
In terms of the Shrinky Dink, what other experiments are currently going on in the lab at the minute?
It’s amazing what you can do with one platform like this. Continuous blood pressure monitors are one of the holy grails of medicine and we’re working on that now using the Shrinky Dinks. Outside of the medical realm, we have used these sensors as controllers for drones. We can put them into a glove and use them to control different things; we’ve made very simple games using these gloves.
We’re also using these sensors to monitor a patient’s movements; when they’re placed on their knees or fingers, the joint angle movement can be measured, which could be used in a lot of different applications. We also have a lot of electrochemical sensing applications that we’re working on right now with this platform, which involves detecting different biological markers etc. In the past we have used the Shrinky Dinks to create very interesting platforms for enhancing fluorescence as well as creating superhydrophobic surfaces.