Finding therapies for Shigella infections

Christina Faherty discusses her work with the pathogen Shigella and her efforts to develop an effective solution for treating infections.
Please can you introduce yourself and provide a brief overview of your research focuses?
I am an assistant professor of pediatrics at the Mucosal Immunology and Biology Research Center (MIBRC) at Massachusetts General Hospital and Harvard Medical School (both MA, USA). My research focuses on bacterial pathogenesis, specifically on pathogens that cause infectious diarrhea. I have worked with several different pathogens such as pathogenic Escherichia coli and Salmonella, but most of my research focuses on Shigella. Our goal is to identify novel targets to develop improved therapeutics and new vaccines, to successfully treat infections.

Why is Shigella infection such a problem?
Shigella is a global infection problem and every year throughout the globe it infects both children and adults in developing and industrialized countries. Large epidemiological studies have shown Shigella is the second leading cause of global diarrheal deaths and the third leading cause of diarrheal death in children under 5 years of age. There is also the problem of antibiotic resistance, to the extent that the World Health Organization has listed Shigella as one of the priority pathogens requiring new treatment therapies in the age of rampant antimicrobial resistance.
How are you utilizing organoid models in your research?
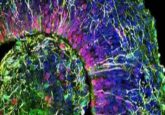
Organoids are a great infection model for us and provide a nice human-specific platform to investigate host-pathogen interactions of the gastrointestinal tract, especially for pathogens like Shigella that are human specific and reliable animal models are lacking. Organoid models allow us to take tissue culture technology and translate it into a more realistic representation of the human cells that are encountered upon infection. We have collaborated with researchers here at the MIBRC, Dr Stefania Senger and Dr Alessio Fasano, who established this model for the center. We have been able to use the model and apply it to our work with Shigella pathogenesis as well as to investigate the other pathogens. We have even done some preclinical analyses to evaluate potential therapeutic strategies that we are interested in trying to further develop.
Based on your research so far, what have you discovered about the effects of Shigella?
For Shigella specifically, we have been able to validate much of the infection paradigm, which is important since most of the previous work has been done using animal models that typically do not produce the usual bloody diarrhea seen in humans. The organoids are a little bit challenging to work with at times, especially from the perspective of pathogenesis research. When organoids are grown in culture, they form spheres and the apical surface of the epithelial cells that the pathogens first encounter is actually on the inside of the sphere. Therefore, a challenging approach to infect the spheroids is to use microinjection systems. Our collaborators were able to help demonstrate that the organoids can be trypsinized to break open the spheres to seed the cells onto a Transwell system. This process helps to create a polarized, single epithelial cell monolayer that has a top (apical) and a bottom (basolateral), which represents the single layer of cells that lines your entire gastrointestinal tract. Through differentiation reagents, we can make sure we are producing mature cells such as enterocytes, mucus producing goblet cells and antigen-sampling M cells that monitor the microenvironment and help initiate the immune response if needed. Interestingly, Shigella exploits M cells so that it can gain access to the basolateral side of the epithelium to invade and enter the cells. With this model, we have been able to detect M cell transit by Shigella, which is interesting and is something we are really excited about. The data helped show that this infection model would be ideal to examine early host-pathogen interactions and to understand infection mechanisms to create successful therapeutics. Shigella invades epithelial cells, tries to stay hidden as long as it can by attempting to regulate the immune response, ultimately aiming to survive long enough to be transmitted to a new host. So, understanding early infection is important.
Does Shigella display specificity in where it imbeds in the gastrointestinal tract?
Shigella is specific to the colon and that leads me to another part of my research: how does the bacteria survive host transit and make it all the way to the colon following oral ingestion to successfully establish infection? The organoids have been established from biopsy samples throughout the intestinal tract. We have models from the duodenum, the end of the small intestine called the terminal ileum, and the colon. We have shown through our analyses that Shigella is specific for the colon. It appears the bacteria have a tissue tropism and we are interested in figuring out why. On a cellular level, the colon is pretty similar to the small intestine, yet Shigella specifically targets the colon. We can see those differences in the model, so we think we are going to be able to answer questions as to why the colon is targeted.
You’ve mentioned that the human specificity has been a challenge of studying Shigella, what other challenges have you come across while you’ve been studying the disease and how are you trying to overcome them?
The organoids really help us get around the fact that there are no adequate animal models for Shigella. Another important consideration is mimicking the host signals the bacteria encounter in the human gastrointestinal tract. Laboratory media does not adequately provide the bacteria with the appropriate host signals that Shigella encounters during gastrointestinal transit. These signals are important for both survival and for the activation of certain virulence factors. Shigella is very efficient: it expresses certain genes at the right time and does not like to waste energy expressing these factors unless needed. So, we’ve tried to mimic what the bacteria encounter as they transition through the small intestine by supplementing laboratory media with bile salts and glucose. Bile is an interesting signal because it is mostly localized to the small intestine, with only 5% entering the colon. For simple sugars like glucose, these signals are available for bacterial utilization as our food is digested. So, it is a nice combination of signals that we can use for these analyses.
All enteric pathogens can resist bile, which typically involves the same mechanisms by which the bacteria resist antibiotics. We found that Shigella, like other pathogens, uses the AcrAB efflux pump to resist bile and that information helps us to understand how Shigella survives host transit to cause infection in the colon. It is intriguing to consider that the same mechanisms are used to resist bile and antibiotics. So, the simple fact that pathogens are exposed to bile essentially helps prime them for an antibiotic resistance phenotype, which has important implications in our current age of antimicrobial resistance. We also demonstrated that the combination of bile salts and glucose induces biofilm formation in Shigella. Biofilms help bacteria to resist harsh environments, so we hypothesize that the biofilm also facilitates Shigella survival and transit through the small intestine. We even mimicked the loss of the bile signal as the bacteria enter the colon and found that the bile signal loss triggers Shigella to disperse the biofilm in a hypervirulent state since infection is greatly enhanced upon this dispersion step. In fact, we are close to publishing results that demonstrate Shigella expresses adherence factors under these conditions. Many people in the field thought Shigella cannot express adherence factors, especially since the structures are not detected following growth in laboratory media. However, when we utilize the media to mimic small intestinal transit, we can see the structures and are able to characterize the genes. These conditions help us to understand how Shigella is using the structures to make initial contact with the epithelial cell surface and we are hoping we now have new therapeutic targets to pursue.
What methods are you using in order to target Shigella infection?
Once we utilize the supplemented media and the organoid infection model, we use several techniques to study pathogenesis such as RNA sequencing or quantitative RT-PCR, and protein expression and mutational analyses. We can evaluate changes in both bacterial gene or protein expression and well as changes in the host cells. Microscopy is also important, ranging from confocal microscopy to electron microscopy, in order to get the detail of either visualizing adherence structures or seeing how the bacterial surface changes, to examining the bacterial-epithelial cell interaction at different time points of infection.
When it comes to trying to tackle the disease, what kind of strategies and techniques are you using to target the infection?
We are hoping we can identify new virulence factors or antigens that can act as potential vaccine targets to generate an antibody response – that would be the ultimate goal. The field has tried for years to successfully develop a Shigella vaccine. Candidates have routinely had problems or been unable to get through clinical trials. We are hoping we can apply new information to develop novel vaccine candidates and get the right formulation that is successful. I also think a very important aspect of new therapeutic development is overcoming antimicrobial resistance. Understanding that bile can trigger an antibiotic resistance-like phenotype is, I think, important for trying to develop new antimicrobials in the future. For Shigella, we need to target the pathogen early enough to prevent the establishment of infection in the colon, and so understanding all the changes that occur during small intestinal transit is important to our future success.
Finally, what really has developed in recent years, and is something that we have started to pursue with collaborators at MIT (MA, USA), is the potential of phage therapy. Phage therapy could give us something that is effective and bridges a gap as the antibiotic resistance problem continues and we try to develop new and successful vaccines.
Why has it been so difficult to create a vaccine? What’s held that area of the research back?
For Shigella specifically, it’s been challenging. A few antibodies have been considered the correlates of protection. When anyone has tried to produce those antibodies with a vaccine, either through injecting live attenuated strains of the bacteria or using some sort of protein and/or lipopolysaccharide formulation to generate an antibody response similar to infection, most of the vaccine candidates have ended up failing. Even if some of the candidates have appeared successful early on, especially in preclinical analyses or safe and well tolerated in early clinical trials, the candidates end up failing during challenge and efficacy studies. The candidates have been reactogenic, especially working with attenuated strains; or the candidates do not provide sufficient protection in challenge studies. In these challenge studies it is difficult to detect differences between someone who has been challenged with infection versus someone who first received a vaccine candidate and was then challenged, so protection is not detected. Shigella infection does not generate an adaptive T-cell response, which is a significant problem for successful vaccine development. In fact, many researchers are trying to figure out how Shigella subverts activation of the T-cell response; an understanding that will certainly go a long way to eventually developing a successful vaccine.
Phage therapy has had a huge boost recently with a successful case, what does this latest development mean for your research?
I think phage therapy offers some great promise. We are at a point where we can see the potential of phage therapy and start pursuing it, whether it is phage therapy by itself or in combination with antibiotics. Phage therapy will provide specific approach to killing the bacteria; or, if used in combinations with antibiotics, can prevent the bacteria from quickly adapting to overcome either the antibiotic or the phage. As I mentioned, we are collaborating with MIT and we are hoping to push phage therapy into a new direction where we can use bioengineering, not only to ensure its success, but also to ensure phages are specific to pathogens. This concept is important for the gastrointestinal tract and the ability to protect the microbiome, where current antibiotics would kill the beneficial bacteria. We are trying to avoid the “total destruction” seen with antibiotics and just specifically target the pathogen in question. Bioengineering will also help to prevent the pathogens from quickly adapting to resist the phage, which has been seen and is a possible challenge for phage therapy. The potential of phage therapy is really important for controlling Shigella infection since it mostly infects malnourished children under the age of five years in the developing world. So, we need therapies that can prevent infection in malnourished children and ensure that we are protecting their microbiome. Malnourished children typically have recurrent diarrhea, which leads to growth and developmental delays that significantly impact developing countries and is very unfortunate. Phage therapy provides a new hope to help both malnourished children and developing countries to truly enhance global health.
What do you think needs to progress with phage therapy before it can become a fully-fledged effective therapy that’s used in common practice?
From what I can see, it seems like researchers are rapidly moving into phage therapies and looking at the potential of phages, especially within the last 5 years. I think efficacy and preclinical analyses will need to be performed to make sure we have the targets right and we have hopefully reduced resistance forming in pathogens. I think it is going to happen at a relatively quick pace, as fast as it can be in science anyway. We can hopefully get phages into early clinical trials and push them along the clinical trial trajectory to see it used as a therapeutic. Researchers are quickly obtaining viable candidates from the lab, so now it is a matter of getting them through clinical trials. There have been several cases around the globe now where patients have been successfully treated with phage, so I think regulatory agencies are very interested in pursuing them as well. Many researchers in the field are at a ”let’s do it” point, especially with the staggering increases in antibiotic resistance.
Shigella is mostly a pediatric disease, is there a particular reason why it seems to be focused on children younger than five?
Well, one of the ideas is that the antibodies that are generated during infection can help to provide protection in adults, at least somewhat partial protection. It could be a scenario where we see mostly children under five because it is their first exposure to Shigella, but that viewpoint might be changing a bit because adults still get infected. It is a matter of whether adults are reporting the infection or whether they are just dealing with the symptoms without going to the doctor.
Interestingly, we have also seen a resurgence of Shigella infection in adults in industrialized nations, across Europe and in the United States. In certain populations, especially in HIV populations of the homosexual community, there are significant rates of transmission of Shigella. We are trying to understand why that is occurring, and it seems to correlate with HIV infection. Researchers in the field are trying to examine the epidemiology associated with this type of Shigella infection. Also, in places like the U.S. and Europe, there are many examples of water-borne or food-borne outbreaks. So, Shigella is transmitting and causing infection. Usually the outbreak reports are triggered when children or adults with additional health complications seek medical treatment. When a child is sick and has watery diarrhea that suddenly shifts to bloody diarrhea, parents quickly take notice and take their child to the pediatrician. However, it will be interesting to see if we can further investigate potential differences in disease patterns or microbiome protection to truly understand why children are more susceptible to infection.
With the HIV association, do you think it is because the HIV weakens the patient making them more likely to feel the effects of the Shigella? Or is there an implication that it might also have a sexually transmitted aspect to it?
There is a sexually transmitted aspect to it, which has been documented. However, it is interesting that it seems to be most the prevalent among patients with HIV, so there could potentially be an important aspect to a weakened immune system that helps Shigella establish infection.