On the hunt for a coronavirus vaccine

Research teams across the globe are using a variety of techniques in a bid to rapidly develop a coronavirus vaccine for the current outbreak.
The release of the genetic sequence of the new coronavirus (2019-nCoV) has resulted in an acceleration of efforts from both pharmaceutical companies and research teams to develop a coronavirus vaccine.
This includes efforts from the NIH (MD, USA), where researchers have modified a section of the virus for use as an antigen, and the Coalition for Epidemic Preparedness Innovations (CEPI; Oslo, Norway), which has committed $11m to three programs led by Inovio Pharmaceuticals (PA, USA), Moderna (MA, USA) and the University of Queensland (Brisbane, Australia). CEPI hopes to have a coronavirus vaccine in production within 16 weeks, although it should be noted that timeframe does not include testing for safety and efficacy.
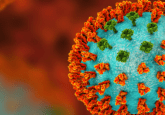
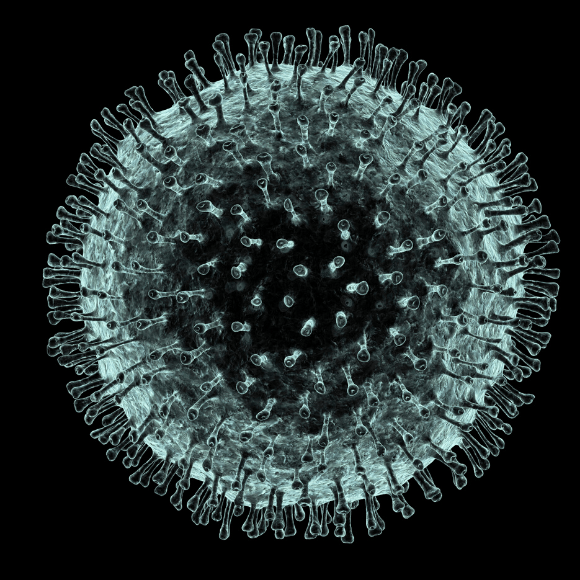
The NIH team has focused on spike proteins, which were originally a focus of investigation during the SARS outbreak in 2001. These proteins dock with a lung membrane receptor called ACE-2 and thus, if the body was able to produce a strong enough antibody defense, it could prevent viral entry to the body. The team had already published work showing stabilizing mutations could be added to the backbone of the spike.
“SARS and the Wuhan coronavirus are similar across 82% of the entire genome. But from a vaccine point of view we were interested only in the spike, which is 70% identical,” explained Kizzmekia Corbett, lead researcher of the NIH coronavirus vaccine team. However, the corona spike protein is a challenge for researchers owing to its size. “One of the reasons it’s so hard to look at is because is (sic) is so big and floppy,” Corbett continued.
The CEPI projects are also building on previous work with the similar virus MERS, and will leverage various platforms already in existence from previous projects. They will also utilize GSK’s pandemic vaccine adjuvant platform technology.
 Diagnosing coronavirus in the lab
Diagnosing coronavirus in the lab
With the coronavirus outbreak spreading, laboratory tests have been developed to allow prompt diagnosis.
CEPI has been working with Inovio’s DNA Medicines platform to develop DNA vaccine candidates against MERS and Lassa fever since April 2018. With this platform they aim to be able to deliver optimized synthetic antigenic genes into cells in order to prompt a robust immune response.
Work at the University of Queensland aims to develop a ‘molecular clamp’ vaccine platform. This aims to synthesize viral surface proteins that can attach to host cells and “clamp them into shape”, making them stable and more visible to the immune system. “We’ve had some extremely promising results so far from trials targeting viruses such as influenza, Ebola, Nipah and MERS coronavirus,” commented Paul Young (University of Queensland).
The Moderna project is seeking to design an mRNA vaccine, and includes a collaboration with the Vaccine Research Center and the National Institute of Allergy and Infectious Diseases (both at the NIH).
“Our intention with this work is to leverage our work on the MERS coronavirus and rapid response platforms to speed up vaccine development. There are no guarantees of success, but we hope this work could provide a significant and important step forward in developing a vaccine for this disease. Our aspiration with these technologies is to bring a new pathogen from gene sequence to clinical testing in 16 weeks – which is significantly shorter than where we are now,” commented Richard Hatchett, CEO of CEPI.
Other efforts include those of Gilead Sciences (CA, USA), which is working with Chinese health authorities to determine whether remdesivir, its experimental drug used to treat the Ebola virus, could be useful for combatting symptoms – they have reported success in treating MERS and SARS in animals.
However, Peter Hotez (Baylor University, TX, USA), noted that it should not be difficult to make a vaccine – the main challenge lies in safety. What’s more, the different approaches each have advantages and disadvantages. “The problem is that is even after manufacturing a vaccine, you still have to go through the safety testing on humans – clinical trials as well as formal toxicology testing in animals. It’s hard to rush and that’s where you tend to get a bottleneck.”