Could carrying multiple copies of antibiotic-resistance genes be a driver of resistance spread?

Carrying multiple copies of antibiotic-resistance genes could be key to resistance spread and evolution in bacteria, particularly those in humans and livestock.
Researchers at Duke University (NC, USA) have identified a significant link between the spread and evolution of antibiotic-resistance genes. In a study published earlier this month, the team at the Lingchong You laboratory found that bacteria exposed to high levels of antibiotics carried multiple copies of antibiotic-resistance genes. Extra copies of resistance genes were often linked to transposons, also known as ‘jumping genes’, that can jump between bacteria and drive the spread of resistance. They also represent an opportunity for the evolution of resistance to novel antibiotics.
Gene duplication is an important step in the evolution of new functions and traits and is a key player in the adaptation of bacteria to different environments; extra copies of a gene not only result in stronger expression but are also free to evolve new functions.
Whilst the duplication of antibiotic-resistance genes following exposure to an antibiotic has been demonstrated previously, few studies have investigated how the vehicles of genetic transfer, like transposons, may drive gene duplication.
“We hypothesized that bacteria under attack from antibiotics would often have multiple copies of protective resistance genes, but until recently we didn’t have the technology to find the smoking gun,” commented Rohan Maddamsetti, first author of the study.
Until now, traditional sequencing methods have made the study of duplication difficult. Because traditional sequencing involves making and counting copies of small bits of genes, it can be difficult to work out whether a high count reflects the quantity of a gene in a sample or whether it has been artificially amplified. Advances in long-read sequencing technologies have allowed researchers to more easily identify repetitive sequences, like gene duplications.
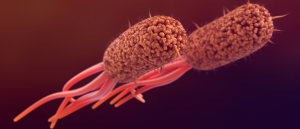 Sharing is caring: how bacteria transfer antibiotic-resistance genes
Sharing is caring: how bacteria transfer antibiotic-resistance genes
Extracellular appendages on gut bacteria accelerate the transfer of antibiotic-resistance genes.
Through mathematical modeling, experimental evolution and genome sequencing, the team at Duke counted the repetitions of antibiotic-resistance genes in samples of bacterial pathogens taken from a variety of sources, including humans, plants and animals, livestock, water and food.
They found that bacteria from sources that are more likely to be exposed to antibiotics, such as humans or livestock, carried multiple copies of antibiotic-resistance genes. Multiple copies of resistance genes were rare in bacteria that were taken from plants and animals, soil and water. Furthermore, higher levels of resistance gene duplication were found in bacteria samples taken from a clinical environment that, again, are likely to have been exposed to antibiotics.
“Most bacteria have some basic antibiotic-resistance genes in them, but we rarely saw them being duplicated out in nature,” reported senior author of the study, Lingchong You. “By contrast, we saw lots of duplication happening in humans and livestock where we’re likely hammering them with antibiotics.”
These findings have important implications for future study of the spread and evolution of antibiotic resistance. In particular, the authors highlight the need for careful examination of the use of antibiotics in hospital and agricultural settings.
“Constantly creating copies of genes for resistance to penicillin, for example, may be the first step toward being able to break down a new kind of drug,” Maddamsetti remarked. “It gives evolution more rolls of the dice to find a special mutation.”
“The majority of antibiotics used in the United States are not used on patients, they’re used in agriculture,” You added. “So this is an especially important message for the livestock industry, which is a major driver of why antibiotic resistance is always out there and becoming more serious.”