How the brain fights off herpes
Herpes’ astronomical abundance and ability to infect nerve cells should regularly lead to devastating infections of the brain, known as herpes encephalitis. But it doesn’t. New research reveals why…
An international research effort – led by Søren Riis Paludan of the Center for Immunology of Viral Infections (Aarhus University, Denmark) and senior researchers at the Memorial Sloan Kettering Cancer Center and Rockefeller University (both NY, USA) – has exposed the mechanism responsible for protecting the brain from potentially deadly herpes infections, using CRISPR screens and a series of other experiments. The research, presented in two papers, provides a vital insight into a little known anti-viral immune response, providing a potential avenue for treatment of the rare instances that herpes can infect the brain and other neurological infections.
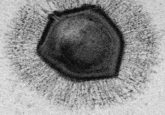
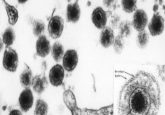
Herpes simplex virus 1 (HSV1) is capable of infecting nerve cells, and infections are near-ubiquitous in humans, with 50–80% of the global population carrying a chronic HSV1 infection. Fortunately, these infections are predominantly symptomless and, when expressed, symptoms are typically mild. Despite its abundance, this neurotropic virus only leads to inflammation of the brain in one in 250,000 cases. When this does occur, however, the infection and subsequent inflammation, known as herpes encephalitis (HSE), can prove lethal.
This set of circumstances raises several key questions. How is the incidence of HSE so low? And what is going wrong in the instances when HSV1 does break through to the brain?
These questions have seemingly been answered by two concurrently published collaborative papers, one led by Paludan [1] and the other by senior authors Lorenz Studer (Memorial Sloan Kettering Cancer Center) and Jean-Laurent Casanova and Shen-Ying Zhang (both Rockefeller University) [2].
 Is a universal influenza vaccine on the horizon?
Is a universal influenza vaccine on the horizon?
Researchers are developing a ‘one and done’ vaccine that will protect individuals against all influenza variants after only one vaccination.
The Studer–Casanova–Zhang paper documents a genome-wide association study of 289 HSE patients to identify potential novel HSE-causing genes. This screen highlighted two unrelated patients with single-nucleotide variants in the highly conserved gene TMEFF1. TMEFF1, the protein produced by this gene, is known to be most abundant and almost exclusively present in the brain.
Using a series of CRISPR screens, depleting TMEFF1 in stem-cell derived human neurons in vitro, and knocking out TMEFF1 in mouse models – in combination with the case study of the two TMEFF1 null patients – the researchers set out to validate the role of TMEFF1 in the protection of the brain against HSE and establish the mechanism through which it does this.
Perhaps most telling was the discovery that the TMEFF1 knock-out mice were more susceptible to HSV1 infection in the brain, but not in the periphery, where TMEFF1 expression is significantly reduced. This finding clearly demonstrated the protective role that TMEFF1 plays in the brain against HSV1 infection.
Collectively, the teams behind these two papers were able to demonstrate that TMEFF1 is not regulated by type 1 interferon, a common innate antiviral molecule responsible for modulating the immune system’s response to viral infection. They revealed that TMEFF1 is instead able to provide this protection by binding to key cell-surface proteins on HSV1, including NECTIN-1 and non-muscle myosin heavy chains IIA and IIB. Through this interaction, TMEFF1 disrupts the function of these proteins, blocking the binding and fusion of the virus with target cells. Importantly, this process bypasses the need for inflammatory signals that could prove self-destructive in the sensitive and tightly packed environment of the brain.
When TMEFF1 is knocked out, HSV1 is able to rapidly enter cortical neurons, leading to the infection and inflammation of the brain and potentially fatal cases of HSE. Commenting on the findings of these papers, Paludan noted that for immunologists the result of this study “illustrates that there are still many immunological mechanisms in the brain that we don’t know about,” and that the research also, “sheds light on how the brain, so to say, prevents unwanted visitors from intruding without causing harm to the brain itself…”
Next, the Aarhus University team hope to investigate whether this is the first of many undiscovered neurological defense mechanisms. Another interesting question to pose is whether TMEFF1, or its inhibition, could play a role in the development of Alzheimer’s, as existing research has highlighted an association between HSV1 infection and the subsequent development of the disease.