How does Zika virus cause microcephaly?
A single Zika virus protein disrupts stem cell connections to cause neural defects in developing fetuses. How does Zika virus cause microcephaly?
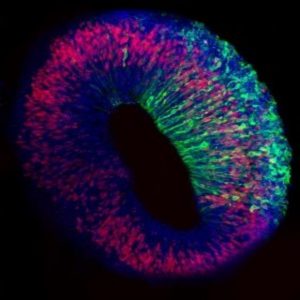
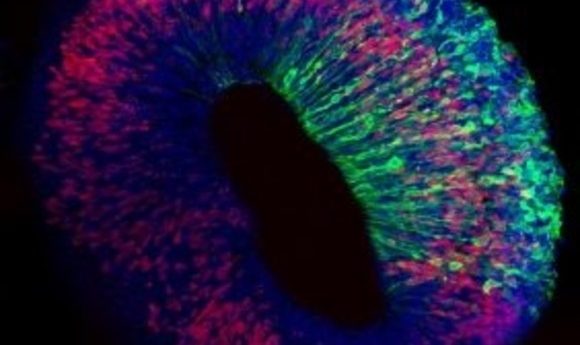
An iPSC-derived brain organoid transfected with a Zika viral protein expression vector. Proliferating radial glial cells (shown in red) and Zika viral protein (shown in green).
Credit: Ki-Jun Yoon and Xuyu Qian, University of Pennsylvania
When first identified in 1947 in the Zika forest of Uganda, the Zika virus raised few concerns, since it caused only mild flu-like symptoms in the adult population. But its recent re-emergence threatened fetuses with the possibility of microcephaly and other neurodevelopmental disorders. Now, Guo-Li Ming from the University of Pennsylvania and her team report in the journal Cell Stem Cell that they have identified the specific Zika virus component responsible for fetal neural defects.
Ming’s team began their study by introducing each of the 10 Zika virus–encoded proteins one-by-one into the brains of mouse fetuses using in-utero electroporation. When they looked at the brains of the resulting mouse pups, they noticed that one protein, NS2A, caused a significant reduction in proliferation, growth, and differentiation of radial glial cells, which are stem cell–generating neural cells that guide the movement of neurons during development. These brains appeared similar to brains infected with intact Zika virus, with reduced neuronal progenitors and disorganized cell polarity in the cortex, along with impaired neuronal migration resulting in an abnormal distribution of neurons.
The researchers next turned their attention to the molecular mechanism behind these abnormalities by identifying several of NS2A’s interacting partners, including some involved in cell-to-cell contact at adherens junctions.
“We focused on adherens junction proteins and found that the protein stability of these are seriously reduced in NS2A infected cells,” said Ki-Jun Yoon from the University of Pennsylvania, first author of the study. “We didn’t realize that Zika virus infection has adherens junction deficits and neuronal progenitor polarity dysfunction.”
Yoon hopes that these findings may lead to therapeutic interventions down the road. “I truly believe that understanding the primary mechanism of disease pathology will be the first step of drug development,” he said. “We can imagine that if we block the interaction between Zika virus NS2A protein and adherens junction protein, we can reduce the symptoms.”