Inflammatory bowel disease and the gut microbiome

Gut bacteria play essential roles in developing and regulating normal immune responses. Can they also help treat autoimmune diseases?
Mammalian gastrointestinal tracts harbor enormous, diverse communities of commensal microbes. Besides playing vital roles in normal physiology, commensal microbiota also help maintain normal immunity, particularly T cell regulation and homeostasis. Studies have shown that germ-free mice lack some subsets of T cells, which also play a central role in many autoimmune diseases like diabetes and colitis.
Now a new study published in Cell demonstrates that a commensal microbe produces a molecule that mimics a human disease-linked autoantigen and protects against colitis by maintaining gut immune homeostasis.
To determine if these gut microbial antigen-reactive T cells migrate to gut in response to colitis, the authors treated mice with a chemical that triggers colitis development. This resulted in an increase of IGRP-reactive CD8+ T cells in the gut. To further assess if the presence of bacterial-epitope reactive T cells contributed to or protected against colitis, they looked at IGRP deficient mice and found resistance to colitis upon the chemical treatment. The results suggest that these autoreactive T cells migrate to the gut and help control colitis by responding to the microbial epitope. Further studies demonstrated that these T cells act by targeting and killing gut dendritic cells.
“We discovered this peculiar population of autoreactive T cells and have been interested in them for about 20 years. Their high prevalence in the peripheral T-cell repertoire and unique phenotypic and molecular features suggested that these cells might exist not to cause diabetes, but rather to protect the host against some other pathology. Thus our hypothesis predicted that these T cells recognized some other antigen in addition to IGRP. We suspected that such an antigen might be encoded in the microbiota,” commented Pere Santamaria from the University of Calgary (Canada), the corresponding author of this study.
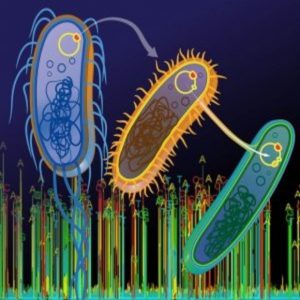
Santamaria and his team first searched the NCBI microbial protein database to find amino acid sequences homologous to mouse IGRP. One of their top hits was an epitope from a family of integrase proteins encoded by Bacteroides, a common species of bacteria found in the gut. The research team next discovered that both mouse IGRP-reactive T cells and human peripheral blood CD8+ T cells recognize this epitope.
To determine if these gut microbial antigen-reactive T cells contributed to, or protected against, inflammatory bowel disease the authors treated mice with a chemical that triggers colitis to develop. This resulted in an increase of IGRP-reactive CD8+ T cells in the gut. They also looked at IGRP-deficient mice and found resistance to colitis upon the chemical treatment. The results suggested that these autoreactive T cells migrate to the gut and help control colitis. Further studies demosntrated that these T cells act by targeting and killing gut dendritic cells.
Santamaria’s team then turned to diabetes and colitis patients, along with healthy volunteers, from whom they collected stool samples for metagenomic sequencing. This confirmed a high prevalence of integrase-expressing Bacteroides in the human gut microbiome.
For Santamaria’s team, these results suggest that cytotoxic T cells against specific microbial epitopes might be useful in treating inflammatory bowel disease. “We are interested in studying how the T cell response to the gut microbiome can be harnessed for therapeutic purposes, as well as in studying if recruitment of these cells to the gut alter the composition of the microbiota,” Santamaria concluded. “In addition, we want to explore in greater detail the effects of this particular bacterial strain on the development of type 1 diabetes.”