Klebsiella pneumoniae: from colonization to infection – an interview with Michael Bachman
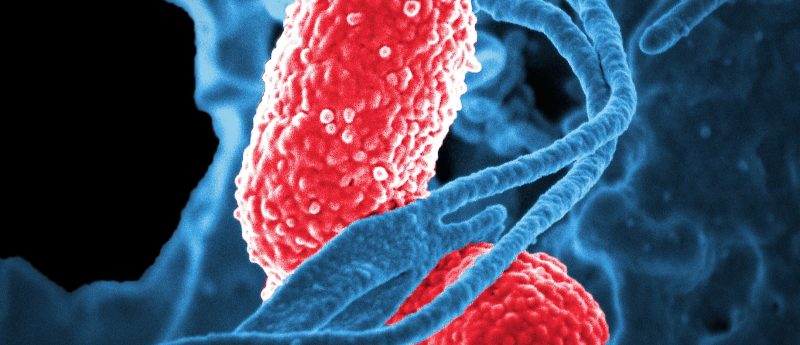
Klebsiella pneumoniae reside in the intestinal tract of approximately 20% of hospitalized individuals but can also cause severe infections – particularly in those who are elderly or immunocompromised. In this interview we speak to Michael Bachman (University of Michigan MI, USA) about his research posing questions around the factors involved in colonization and infection, and whether these could be used to stratify high-risk patients in the future.
First, can you introduce yourself and tell us a bit about your background?
My training started with a combined MD–PhD program at University of Michigan studying Legionella pneumophila. Then, once I finished medical school, I did a residency in clinical pathology, a fellowship in clinical microbiology and then a postdoctoral fellowship where I started studying K. pneumoniae. I’m now at University of Michigan again where I am the Associate Director of the Clinical Microbiology Laboratory. My research laboratory at the university is focused on K. pneumoniae and trying to identify risk factors for infection in colonized patients.
Could outline the work you are presenting here at ASM Microbe (20–24 June 2019, CA, USA)?
So, we have two sets of work that we are doing but the primary focus of the lab is K. pneumoniae. What we had done in some pilot work was ask, what is the association between intestinal colonization and subsequent infections for K. pneumoniae? The data that supported that link was about 45 years old at the point we did the study and the epidemiology of infections in the hospital had shifted from being predominately Gram-negative to predominantly Gram-positive, so we wanted to see what the strength of association currently is.
We looked at a cohort of intensive care unit patients who were being screening for vancomycin-resistant enterococci and then we used those residual samples to screen for Klebsiella, discovering that there is a significant rate of colonization. Moreover, we saw that there is a significant and independent association between colonization and subsequent infection.
“The question that we are really pursuing now is, how can you stratify that risk?”
The question that we are really pursuing now is, how can you stratify that risk? We know that there is a lot of variability in the patients and their underlying conditions that might increase the risk of developing an infection, but we also know that Klebsiella has a lot of genetic diversity – if you compare any two isolates coming out of the clinical laboratory their genome content might differ by as much as about 20% or approximately 1000 genes. So, our hypothesis is that there are genes circulating within the species that are associated with an increased risk of progression from colonization to disease, and we are trying to find those risk factors. That is the primary focus of what we are working on and what we are presenting here.
We also have different research questions trying to use some of the approaches from the clinical microbiology laboratory to investigate associations between contents of the microbiome and subsequent infections, particularly sepsis, and Enterobacteriaceae infections more broadly. In that work too there is this link between what is going on in the intestine and the infection.
Why do you think Klebsiella is an area of unmet need?
Klebsiella is one of the most common causes of healthcare-associated infections and it is also the most common species that has carbapenemase production in the Enterobacteriaceae family –a family of Gram-negative pathogens including E. coli, Klebsiella and others – so I really feel like it is one of the most urgent threats in terms of antimicrobial resistance. There has been a lot of focus on understanding carbapenemase production and exploring the particular lineages that are associated with carbapenemase-encoding plasmids but the unmet need is that we really have a poor understanding of how Klebsiella as a species actually causes infection in the first place.
That’s why our approach is to really take a step back, look at the species level and ask what the mechanisms are by which patients get infected, then hopefully we can apply those insights to the carbapenemase-producing strains as a subset of that larger population. I think that is really the need because not a lot of people really asking questions about pathogenesis of the bacteria.
You talked about colonization and identifying which patients might be at highest risk – do you think eventually that data could be used for infection prevention?
If there are ways to prevent the infection in the first place, I think that is a powerful approach.
This is what I think the real promise of this work could be because I think that while we are developing some new antibiotics, with antibiotics typically there is already resistance in the environment. If there are ways to prevent the infection in the first place, I think that is a powerful approach. What I am hoping is that as we develop predictive models and the ability to stratify the risk in these patients this knowledge could be partnered with other work looking at ways that you can manipulate the microbiome and perhaps eliminate colonization with Klebsiella or more broadly with the Enterobacteriaceae family that includes Klebsiella.
I think that what we can do today is maybe somewhat limited, you might be able to do susceptibility testing in a patient at high risk and guide empiric therapy or there maybe are some current infection prevention techniques that might be triggered, but I think the promise is probably as we develop novel approaches to manipulate the microbiome and clear unwanted organisms, that this could be applied to this data.
You might also like: