Novel parasites and understanding parasite–host interactions – an interview with Sandra Maruyama
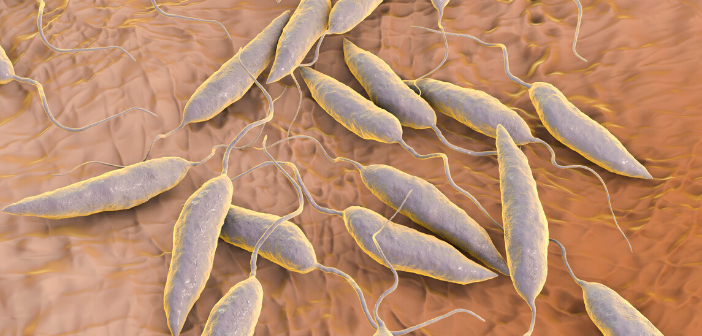
In October 2019 researchers from Brazil identified a new parasite, which presented with similar symptoms to visceral leishmaniasis. To discover more about this novel parasite and other parasitic diseases in Brazil, we interviewed Sandra Maruyama from the Federal University of São Carlos (UFSCar; São Paulo, Brazil) about her research and the future of this field.
First, could you introduce yourself and give a brief summary your career to date?
I am biologist by training (2005) and mother of two little girls. My academic background was entirely obtained from Brazilian public universities. I earned my Master’s (2008) and PhD (2012) degrees both in basic and applied immunology from Ribeirão Preto School of Medicine, University of São Paulo (USP). During my graduation period I performed research projects to study host–parasite interactions through transcriptomics and reverse vaccinology, using the cattle tick as an ectoparasite. During my first post-doc at USP, I spent 1 year (2013) as visiting researcher in the functional genomics team from European Bioinformatics Institute (EMBL-EBI) in Hinxton, UK. In 2014, I was still at USP as I started a second post-doc, when I decided to apply my ‘omics’ background to study leishmaniasis too.
Between 2015 and 2017, I was an assistant professor hired by UFSCar to teach genetics, molecular biology, immunology and bioinformatics in undergraduate courses. Meanwhile, I applied to Young Investigator Award (JP) of São Paulo Research Foundation (FAPESP), which is an award granted to early-career investigators to create a new research group. I was awarded with the JP grant in July 2017 and since then I am a Visiting Researcher at the Department of Genetics and Evolution from UFSCar. More information can be viewed through my ORCID iD: https://orcid.org/0000-0001-6807-1452
Could you give us an overview of your research?
“Through whole-genome sequencing, we aim to characterize the parasite’s genetic diversity from an endemic region in Northeast Brazil and trying to associate this diversity with different responses to treatment and disease outcomes.”
Currently, my research uses genomics approaches to study Leishmania and leishmaniasis. The project presents two branches: functional genomics of visceral leishmaniasis and comparative genomics of Leishmania parasites. Through RNA-seq analyses of blood samples from visceral leishmaniasis (VL) patients (before and after treatment), asymptomatic individuals (positive serology for Leishmania infection, but without clinical signs) and healthy individuals (controls), we aim to identify molecular mechanisms involved in different outcomes of infection. Through whole-genome sequencing (WGS), we aim to characterize the parasite’s genetic diversity from an endemic region in Northeast Brazil (Aracaju, Sergipe) and trying to associate this diversity with different responses to treatment and disease outcomes. Our young group hope to contribute with insights and findings for better understanding of the host–parasite interaction in visceral leishmaniasis in Brazil.
What can genomics tell us about visceral leishmaniasis and other parasites?
Genome analyses are powerful to provide molecular landscapes of visceral leishmaniasis and will be helpful to pinpoint biological pathways underlying the pathological processes triggered by Leishmania infection. Interestingly, in VL approximately 80% of infected people are asymptomatic (resistant to parasite?) and the remaining 20% presents a range of clinical forms from oligosymptomatic to severe disease, with a lethality rate of 6%. By identifying the molecular processes encompassed in immune responses of these different outcomes, functional genomics contributes to understand the mechanisms implicated in control of Leishmania infection and progression of disease.
Furthermore, comparative genomics and population genomics of clinical isolates from VL patients are useful for public health agencies to develop programs related to molecular surveillance, epidemiological studies, efficacy of available treatments, disease control and also the discovery of new drugs. By this way, many other parasitic diseases can be benefit from genomics approaches for a comprehensive understanding of parasite infection.
How important is understanding the parasite–host interaction?
In the parasite–host interaction, factors from both sides drive the relationship between them. An exacerbated host immune response might kill parasites, but the side effects can result in injuries, disorders and even death. The damage caused by a highly pathogenic strain of a parasite may also lead to host’s death, and then it is the end of line. It is important to know how the infection is controlled by an efficient immune response and how the parasites subvert from host’s responses; extreme reactions of both sides of any interaction are not good.
“Understanding how the balance is kept by both organisms can reveal the forces that play roles during co-evolution process…”
So, understanding how the balance is kept by both organisms can reveal the forces that play roles during co-evolution process and this ‘basic knowledge’ can provide key elements to identify biological markers that will be important not only for the improvement of current diagnostic and treatment, but also to development of new drugs, treatment options, prognostic markers, vaccines and more accurate and fast diagnostic methods. Additionally, in leishmaniasis we also have other complex interactions to be understand, such as those of Leishmania with vectors and reservoir animals.
You recently published a paper outlining the identification of a non-leishmania parasite in Brazil – what further research is needed to understand this species?
This unknown species was isolated from a fatal case of VL, which presented very atypical clinical manifestations, besides recidivism and refractoriness to treatment. Because of severity of the case, we decide to study the parasite strain. Initially, we thought that could be a very pathogenic strain of Leishmania infantum, but classical molecular approaches for typing of Leishmania species always failed. Surprisingly, with the WGS analysis we discovered that the parasite isolated (LHV60 strain) from the fatal case was not Leishmania, but a Crithidia-related parasite instead.
This was one case; a long pathway is open ahead. Now, it is efforts are necessary to promote extensive surveys through molecular epidemiology to understand the distribution and prevalence of this new parasite; identify vectors and reservoir animals; develop differential diagnostic and also proper treatment (new drugs?). A lot of studies will be necessary to characterize the life cycle of this new parasite and compare it to Leishmania; how is the amastigote intracellular infection, how is the interaction with the vector, how is a co-infection scenario. A central question that arises is whether the parasite can solely cause a leishmaniasis-like disease (that would be consequently a new disease) or it worsens the Leishmania infection, leading to a severe form of visceral leishmaniasis.
In the past years, researchers from the University Hospital of Sergipe in Aracaju, who collaborate with my group, have observed an increasing number of patients diagnosed with VL and many of them are refractory to conventional treatment. Since 2012, some clinical isolates, presumably of Leishmania, obtained from VL patients attended at University Hospital have been cryopreserved. Because of this finding of non-Leishmania parasite in a VL case, we recently started to type these other samples by PCR (using the markers SSU – 18S small subunit RNA and gGAPDH – glycosomal glyceraldehyde-3-phosphate dehydrogenase) and the preliminary results have shown that the majority of clinical isolates analyzed so far have presented with sequence identity to the LVH60 strain. Patients have been treated to Leishmania infection, but they were infected, or perhaps co-infected, with another parasite. To understand what is happening, we also need to analyze samples straightway from the patient’s tissues, but unfortunately only few VL patients presented paired samples, i.e., parasite isolate and tissues from the same patient. Most recently, efforts have been done to collect informative samples to uncover this new parasite and the outcome of infection or co-infection.
Where do you hope to see this field in 5–10 years’ time?
Molecular parasitology will be continuing to advance, providing significant findings and knowledge that will be important to public health agencies worldwide to plan and implement measures related to treatment, control and prevention of parasitic diseases, as well as be vigilant to the emergence of new parasites or pathogenic strains of currently known parasites. Genomic surveillance for parasitic diseases will be an important strategy for understanding and to fight against neglected tropical diseases and I hope that private and public/government research agencies increasingly support and encourage this kind of approach in coming years.
Finally, any other comments you would like to add?
“The global rise of temperatures may not only support the increase and spread of known infectious diseases, such as dengue, malaria, African trypanosomiasis, Chagas disease and leishmaniasis to new areas, but also it can be favorable to the emergence of new pathogens.”
It is known that the climate changes have significant impacts on burdens of vector-borne diseases. The global rise of temperatures may not only support the increase and spread of known infectious diseases, such as dengue, malaria, African trypanosomiasis, Chagas disease and leishmaniasis to new areas, but also it can be favorable to the emergence of new pathogens. Global warming over the years might be selecting arthropod-exclusive parasites (such as monoxenous trypanosomatids) that became tolerant to high temperatures and this could enable these parasites to survive at human body temperature, causing an opportunistic disease or worsening a pre-existing disease. Thus, it is important pay attention as to whether reports of monoxenous trypanosomatids found in humans are merely opportunist or if they have the potential to threaten public health.
You might also like: