Two-pronged strategy boosts mRNA COVID-19 vaccines

Researchers have modified COVID-19 vaccines to produce a stronger immune response in mice.
RNA COVID-19 vaccines have proven effective at reducing the severity of infection, but reducing costs would make them more accessible. Now, a team of researchers from Massachusetts Institute of Technology (MIT; MA, USA) have found a potential way to do this by engineering the vaccines to produce a stronger immune response, reducing the dosage required. The strategy could be used for other RNA vaccines in development, for example for cancer.
RNA vaccines use a strand of RNA to encode a viral or bacterial antigen. For COVID-19 vaccines, the RNA strand codes for a part of the virus’s spike protein. The RNA is packaged in a lipid nanoparticle carrier, which shields the RNA and helps it enter cells. Once inside cells, the RNA is translated into proteins that trigger the immune system to produce antibodies and T cells that respond in the event of a COVID-19 infection. Although the original COVID-19 RNA vaccines produced a strong immune response, the MIT team wanted to see if they could make them more effective using adjuvants.
 FDA funds research into first continuous mRNA-manufacturing platform
FDA funds research into first continuous mRNA-manufacturing platform
A 3-year research program, funded by the FDA, aims to design the first continuous mRNA-manufacturing platform.
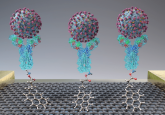
To do this, the researchers took a two-pronged approach, by modifying both the antigen and the lipid nanoparticle that delivers it. First, they focused on C3d, a protein that binds to antigens and amplifies the antibody response to those antigens. They engineered the mRNA to encode the C3d protein fused to the antigen, meaning both components are produced as one protein.
In the second phase of their strategy, which focused on the lipid nanoparticle carrier, the researchers created a library of 480 lipid nanoparticles with different chemistries. They then evaluated the nanoparticles and identified the ones that boosted the response.
“We understood that nanoparticles themselves could be immunostimulatory, but we weren’t quite sure what the chemistry was that was needed to optimize that response. So instead of trying to make the perfect one, we made a library and evaluated them, and through that we identified some chemistries that seemed to improve their response,” explained senior author Daniel Anderson.
The team tested their vaccine in mice and found that the mice given the adjuvanted vaccine produced ten-times more antibodies than those given an unadjuvanted vaccine. The adjuvanted vaccines also elicited a stronger response among T cells.
“For the first time, we’ve demonstrated a synergistic boost in immune responses by engineering both the RNA and its delivery vehicles,” first author Bowen Li commented. “This prompted us to investigate the feasibility of administering this new RNA vaccine platform intranasally, considering the challenges presented by the mucociliary blanket barrier in the upper airways.”
They found the vaccine had a similarly strong immune response in the mice when delivered intranasally. If developed for use in people, an intranasal vaccine could offer enhanced protection against COVID-19 infection by generating an immune response in mucus membranes. It would also be easier to administer.
If developed further, this strategy could help reduce the dosage and cost of the mRNA COVID-19 vaccines, making them more accessible. The MIT team is now exploring whether their two-pronged strategy could be used to help boost other types of RNA vaccines, such as cancer vaccines.