West Nile virus: MRI scans uncover evidence of long-term neurological damage
Imaging of individuals with a history of West Nile virus (WNV) infection has uncovered that many – including those with mild or no symptoms – had evidence of brain damage years after the original infection, according to research presented at the American Society of Tropical Medicine and Hygiene (ASTMH) Annual Meeting (5–9 November, Baltimore, MD, USA).
The Centers for Disease Control and Prevention (GA, USA) has documented over 2000 mortalities resulting from WNV infection, however it has been suggested that this may be higher – particularly if individuals infected with WNV die many years after infection.
This study, from researchers at the Baylor College of Medicine (TX, USA), was carried out over 10 years, representing one of the largest assessments to track neurological complications in WNV patients, moreover, it is the first to link complications, including memory impairments and tremors, to physical evidence of brain damage.
Lead author, Kristy Murray (Baylor College of Medicine) commented: “Our findings add to a growing amount of evidence that West Nile virus is a serious health threat that deserves considerably more attention because there still are no drugs available to treat it and no vaccines to prevent it.”
The study, carried out in in Houston (TX, USA) from 2002–2012, tracked 262 individuals with a history of WNV, monitoring them for evidence of long-term problems. From this group, 117 were tested for neurological deficits, revealing that 49% of these possessed some type of abnormality. The most common physical problems reported included abnormal reflexes, muscle weakness and tremors, in addition, several participants’ demonstrated signs of cognitive impairments beyond that expected from age-related decline.
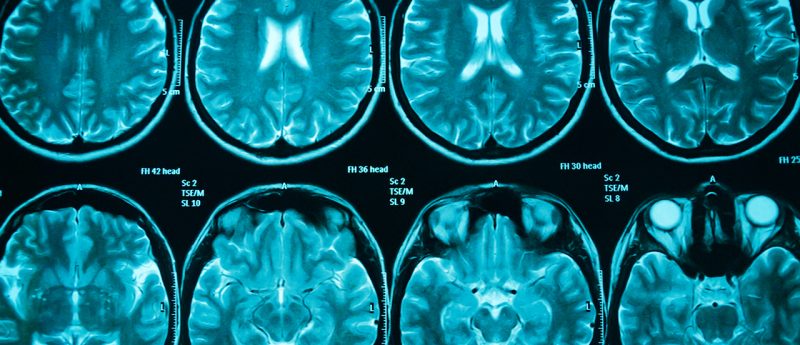
Of the participants suffering abnormalities, 30 individuals agreed to assessment via MRI imaging, revealing damage and thinning in different parts of the cerebral cortex. The team also discovered that in individuals where WNV had progressed to neuroinvasive disease, the scans showed signs of degeneration or atrophy in several regions of the brain, including the cerebellum and the thalamus.
“The issues we are seeing on the MRIs are consistent with what would occur from an infection that caused a lot of inflammation in the brain,” Murray explained. “Inflammation can lead to scarring as the brain starts to heal, and that scarring can cause damage.”
However, the researchers also discovered that evidence of neurological disorders and injury was not constrained to neuroinvasive infections but was found across the whole spectrum of disease, including seven participants who had experienced no symptoms at all but whose infection was discovered via routine screening.
Co-author Shannon Ronca (Baylor College of Medicine) stated: “It will be important to regularly assess people who have been infected with West Nile virus for early signs of neurological deficits and brain MRIs should be considered when symptoms are observed.”
With author Patricia Walker (Baylor College of Medicine) concluding: “It’s critical for our scientists to keep following the outcomes for patients who have suffered a West Nile virus infection so that we have a full picture of the dangers posed by this disease. The risks they are uncovering highlight the need to intensify prevention efforts, from mosquito control to developing a protective vaccine.”
Source: www.eurekalert.org/pub_releases/2017-11/b-mow110117.php