Ray Owens on nanobody technology for use against SARS-CoV-2
As an expert in biotechnology and biochemistry, Ray Owens spoke to Editor Lucy Chard on the use of nanobodies from llamas as a platform for binding to the spike protein on the surface of the SARS-CoV-2 virus.
Biography: Ray Owens completed his PhD in the Department of Biochemistry, University of Cambridge (UK) on the biosynthesis of plant cell wall glycoproteins. Following post-doctoral work in London and Oxford (both UK), he joined the UK Biotechnology company, Celltech (Slough, UK) and worked on antibody engineering and small molecule drug discovery programs. In 2002, Ray Owens returned to Oxford University where he developed a structural proteomics facility to support high throughput structural biology. He is currently Head of Protein Production UK at the Rosalind Franklin Institute on the Harwell Science Campus near Oxford (UK).
Can you give a brief background of your career to date?
I am Professor of Molecular Biology at the University of Oxford. My background is in biochemistry and biotechnology and I’ve worked in both industry and academic labs. My main focus has been an interest in proteins; how we make them and how we study their structure and function.
Your work has been in the news recently regarding nanobodies and the SARS-CoV-2 virus – could you give an overview of this work?
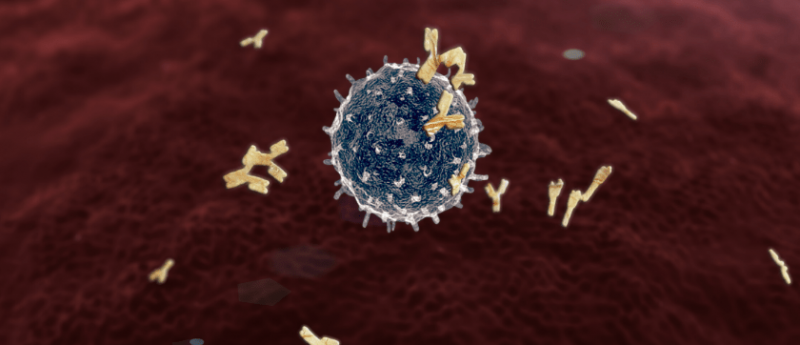
Nanobodies are small single-domain antibodies that can be used as targeting agents with numerous applications in the biomedical sciences, including diagnostics and imaging. We have been developing a technology platform to derive binding agents – nanobodies – to SARS-CoV-2 proteins, particularly focused on the so called ‘spike protein’, which is the viral protein which interacts with the human cells and is the first step in driving infection. Clearly, from work on many other viruses, antibodies that interact either to intercept or bind the spike protein can block entry into the cell. What we have been able to do is to use nanobodies to probe the structure of the spike and see if we can block that interaction.
Practically, what we have done is to use a library of these small domain proteins that are presented on a bacteria phage as a library of some 10 million or more individual/unique binding agents, derived initially from the immune cells of the llama (Lama glama). Camelids and llamas are unique in that part of their immune response to foreign antigens is to produce antibodies that do not have a light-chain. These heavy-chain only antibodies comprise a constant region and a variable domain – VHH (variable heavy heavy) – that is the unit we are using to probe the structure of the viral proteins. We have been making parts of the spike protein in mammalian cells as recombinant proteins using the sequence of the viral genome as a template. We then use these as probes to fish out from our library individual VHHs, that specifically bind to the spike protein. Once we know the sequence of these binders, we have been able to engineer them to improve their binding ability.
How many VHHs have you been able to extract using this technique?
What we find is that the DNA sequences of the VHHs fall into different classes so we have about a dozen clusters of sequence-based unique binders; we have been characterizing these progressively and have been improving their affinity for interaction with the virus.
What key factors made this breakthrough possible in such a short space of time?
I would highlight two things; firstly, we were pre-prepared, as we had identified this nanobody technology platform as something we needed to have within the Franklin. We have been setting this up for over a year, working up the methodology and trialing it so that when SARS-CoV-2 came along it was obvious to apply that platform technology to binders of the virus. The second factor has been the global sharing of information, the sequence of the virus was made available very quickly and once we knew the sequence of the virus then we could interpret that in order to produce the different component proteins.
You are making this research available to the University of Oxford; how do you hope to collaborate with them to use this technology to combat the pandemic?
The collaboration is ongoing and what we use these binders for is to investigate the structure of the actual spike protein. Working with colleagues in Oxford and also the Diamond Light Source (Oxford, UK), using the electron microscopes there, we have now got information on where the nanobodies bind to the spike protein, which is providing us with insights into their activity. We are collaborating with other groups in Oxford who have been looking at model systems for studying the interaction between the virus and cells. The ambition here is to demonstrate that nanobodies are not only useful tools to investigate the properties and structure of the virus but have the potential to be used therapeutically by blocking the virus entry into cells.
Do you think this research could be useful in the future to prevent similar outbreaks?
I hope so! The technology would be applicable to similar coronaviruses/viruses – it’s generic. What we are learning is that the COVID-19 situation is not going to resolve quickly, and I think that this will hopefully catalyze a longer-term investment in research around coronaviruses in general. There are tools that we have generated that will have applications beyond the immediate experiments that we are doing and the protocols will hopefully be of use in the study of other viruses.
Finally, what positive changes have you seen in the scientific community in light of these unprecedented times and do you think these will continue once we move forward from this disease?
The speed with which things have moved has been incredible and this is credit to the fact that people have been willing to share very early data that’s not been published or peer reviewed, just to make it available within the community. It’s certainly a unique situation and this global collaborative spirit that has gone around shows that people have seen the importance of working together so it has become a high priority and we’ve seen a real readiness to embrace that. Colleagues have very quickly switched from working on their own projects to focusing entirely on COVID-19, applying their experience and technologies to the working on the SARS-CoV-2 virus.
Any final comments?
I am involved in a distributed research infrastructure for structural biology, called Instruct-ERIC, that links together a number of laboratories across Europe all of whom are focusing on COVID-19 research. As a transnational organization, Instruct-ERIC helps to bring people into contact and provides access to shared expertise and technology, which is really important in the current crisis.
The opinions expressed in this feature are those of the interviewee and do not necessarily reflect the views of The Nanomed Zone or Future Science Group.
For further updates regarding the pandemic, visit our dedicated COVID-19 Hub here.
For more nanomedicine updates straight to your inbox, become a member of The Nanomed Zone here.





