Nanocarriers could enhance longevity of type 1 diabetes treatment

Researchers have developed a nanocarrier to improve the effectiveness of pancreatic islet transplantation, which is a potential cure for type 1 diabetes.
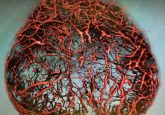
In type 1 diabetes, the immune system attacks pancreatic islets, which are comprised of cells that control insulin production. As sugar levels in the blood increase, beta cells within pancreatic islets should respond and release insulin to curb blood glucose levels. However, in type 1 diabetes, the beta cells’ functionality is lost; therefore, regular insulin injections are needed. Over the last few decades, pancreatic islet transplantation has been developed as a promising cure for type 1 diabetes; however, these transplanted islets are eventually rejected by the immune system.
Current immunosuppressants, including rapamycin, do not protect these transplanted pancreatic islets, and result in several side effects. “To avoid the broad side effects of rapamycin during treatment, the drug is typically given at low dosages and via specific routes of administration, mainly orally,” explains Evan Scott who leads the research team at Northwestern University (IL, USA) developing new techniques for more effective immunomodulation. “But in the case of a transplant, you have to give enough rapamycin to systematically suppress T cells, which can have significant side effects like hair loss, mouth sores and an overall weakened immune system.”
The researchers developed nanocarriers to deliver rapamycin and prevent this wider immune response that shuts down T cells without specificity. Instead of targeting T cells (the therapeutic target of rapamycin), these nanocarriers are designed to specifically target and modify antigen presenting cells, resulting in more directed immunosuppression. Scott explains, “by changing the cell types that are targeted, we actually changed the way that immunosuppression was achieved.”
 New supermolecule could revolutionize artificial protein synthesis
New supermolecule could revolutionize artificial protein synthesis
Researchers synthesize the first supermolecule with a chemically bonded DNA helix and peptide by changing the chirality of the peptide structure.
Rapamycin is normally orally administered; however, with this nanodelivery method can be subcutaneously injected into fatty tissue. This uses a different metabolic pathway so drug loss in the liver is minimized, meaning only around half the standard dose of rapamycin is needed.
This new formulation was tested in mice and compared to the standard Rapamune® oral administration after an islet transplantation. The mice were injected every 3 days for 2 weeks and were observed to have minimal side effects, as well as being cured of diabetes for the 100-day trial. The research team believes these results should last the entirety of the transplanted pancreatic islets’ life.
Whilst using nanodelivery methods to minimize the side effects of drugs is not new, Scott highlights that “we’re not enhancing an effect, we are changing it – by repurposing the biochemical pathway of a drug, in this case mTOR [the mammalian target of rapamycin] inhibition by rapamycin, we are generating a totally different cellular response.”
The importance of this study is close to home as Jacqueline Burke, the first author of the study, was diagnosed with type 1 diabetes at the age of nine and has always wanted to work in, and contribute to, diabetes research. “At my past program, I worked on wound healing for diabetic foot ulcers, which are a complication of type 1 diabetes,” Burke said. “As someone who’s 26, I never really want to get there, so I felt like a better strategy would be to focus on how we can treat diabetes now in a more succinct way that mimics the natural occurrences of a non-diabetic person.” This combination of pancreatic islet transplants and enhanced immunosuppression could do just that.
The research team hopes this nanocarrier technology can also be applied to avoid the rejection of other transplanted tissues and organs and are working towards the clinical application of this technology in type 1 diabetes patients.