Fetal benefits of treating opioid use disorder during pregnancy are confirmed
Refer a colleague
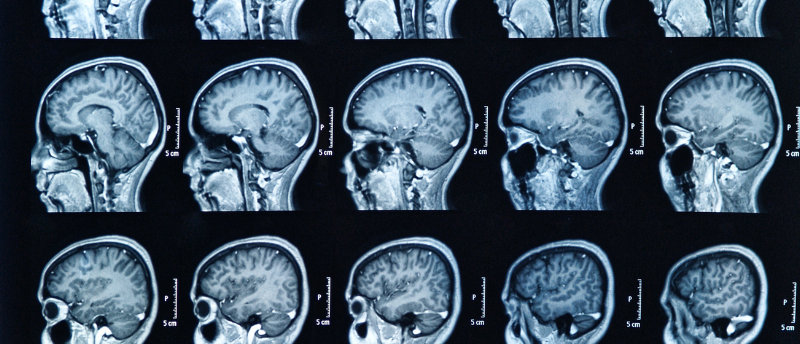
Researchers used emergent MRI technology to understand the impact of prenatal opioid exposure on early brain development and the neural mechanism behind current medications.
“Choose life. Choose a job. Choose a career. Choose a family…” muses Mark Renton in Trainspotting’s opening monologue, finishing on Irvine Welsh’s characteristic bleak mockery: “But why would I want to do a thing like that?” Fast forward two and a half decades and the opioid crisis in the USA is tragically distant from the choose-your-own-destruction of 1990s grunge-adjacent counterculture portrayed in Trainspotting.
In 1999 the prevalence of opioid use disorder in pregnant women in the USA was 1.5 per 1000 delivery hospitalizations, which are hospital stays due to maternal care rather than infant complications. By 2014 that number was 6.5 per 1000 – a quadrupling in the rate.†
“We are in a nationwide opioid crisis, so there’s an urgent need for us to better understand how opioid exposure in pregnant women impacts their children,” observed Wei Gao, the senior author of this study validating the benefits of opioid use disorder medications during pregnancy (Cedars-Sinai; CA, USA). “Using imaging techniques can help us identify the risks as early as possible so that we can hopefully intervene and minimize the potential adverse impacts on the developing fetal brain.”
Abnormalities associated with prenatal opioid/other drug exposure (PODE) in infants less than 1-month-old exceed alterations associated with exposure to drugs excluding opioids. This exposure leads to a considerable impact on neurotransmitter-receptor signaling during fetal development, with the most prominent changes occurring in reward-related frontal-sensory connectivity.
Treating opioid use disorder in expectant women can reduce the risk of opioid-related brain abnormalities in infants; however, the mechanisms behind these medications are not well understood. Numerous studies have investigated the subject, with little revealed about how opioid exposure-stabilizing medications such as buprenorphine or methadone work.
 A diagnostic test for ALS could finally be on its way
A diagnostic test for ALS could finally be on its way
Amyotrophic lateral sclerosis could soon be diagnosed from a muscle biopsy as researchers identify a possible biomarker in muscle tissue.
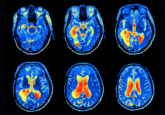
To unpack those questions, the researchers of this study utilized advanced resting-state functional MRI imaging to compare the brains of 109 2-week-old babies. This non-invasive neural technique allowed the researchers to observe communications between different regions of the brain.
“The data from the scans is in a time series of activity from every area of the brain. We are able to use this data to compare the series between the two brain areas to see just how synchronized their activities are,” explained first author Janelle Liu.
Of the 109 infants studied, 42 were prenatally exposed to opioids or other drugs, 39 were prenatally exposed to drugs but not opioids, and 28 were drug-free controls. To determine the effects of medication for opioid-exposed neonates, the 42 infants were further divided into those who had received treatments, 31 in total, and the remaining 11 who had not received treatment.
The findings confirm what scientists had suspected: that prenatal opioid exposure has significant effects on the functional connectivity of the brain, impacting regions responsible for reward processing and emotional development. The fMRI imaging also revealed improvements in brain function following treatment.
This research indicates that, while not capable of undoing the damage to neural connectivity, these medications can help to treat aberrations to connectivity, underlining the importance of treatment during pregnancy for infant brain development.
The researchers will continue this work by pairing their findings with environmental conditions, with which they hope to improve the treatment efficacy.
Please enter your username and password below, if you are not yet a member of BioTechniques remember you can register for free.