Understanding the role of APOE genotype on brain function
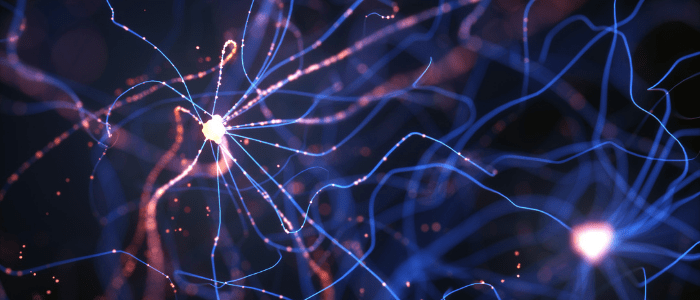
Researchers have investigated the relative effect on the brain of different genotypes of APOE, a known genetic risk factor for late-onset Alzheimer’s disease.
While the causal factor for Alzheimer’s disease remains unknown, many factors both environmental and genetic have been associated with the disease. The APOE gene has long been known as the greatest genetic risk factor for late-onset Alzheimer’s disease, with its different variants posing different levels of risk for disease development. There are three different variants of the gene, the most common of which – APOE3 – comes with an average risk of developing Alzheimer’s disease. However, APOE4 and APOE2 each come with a higher and lower risk of Alzheimer’s risk, respectively.
Though the relationship to disease risk is well understood, the effect of each variant on early brain function and disease development has remained elusive. Many of the studies into the role of APOE have been conducted on clinically diagnosed Alzheimer’s disease patients or elderly APOE4 carriers, with little research conducted on young, healthy individuals. A recent study, led by researchers at the German Center for Neurodegenerative Diseases (DZNE; Bonn, Germany), sought to investigate the effect of APOE4 in young brains and discover how it may relate to early Alzheimer’s disease processes.
The study involved 82 participants with an average age of 20 years old. According to their APOE genotype, 33 had an average risk of developing Alzheimer’s disease in later life, 34 had an increased risk and 15 had a reduced risk. All participants underwent functional MRI (fMRI) scans, during which they were asked to perform a pattern separation task. During the task, they were shown 150 successive images of everyday objects and they were required to identify whether the image was new or if they had seen it before and, if they had, whether its position had changed.
 Can a hormone replacement protect women against Alzheimer’s disease?
Can a hormone replacement protect women against Alzheimer’s disease?
Two-thirds of those with Alzheimer’s disease are women. With risk factors such as hormone levels and reproductive stage at play in postmenopausal women, researchers suggest an estrogen replacement may prevent Alzheimer’s onset.
Blood-oxygen-level-dependent fMRI measured the brain activity of individuals as they performed the task, with the hippocampus – a key brain region for memory production and one of the first areas affected by Alzheimer’s – being focused on as the region of interest. The scanner used had a magnetic field strength of 7 Tesla, allowing the researchers to view distinct sub-regions of the hippocampus with a great level of detail.
The researchers found that all participants performed equally well on the pattern separation task, as would be expected for young and healthy individuals. However, there were differences in brain activity depending on their APOE genotype, suggesting that the different variants influence how the brain responds to memory formation and retrieval. A difference was noted not only between those with average and increased risk of developing Alzheimer’s, but also in those with average and reduced risk.
It is as yet unclear whether the present results are significant for the development of Alzheimer’s in later life; however, they do demonstrate that genetic risk for Alzheimer’s disease can alter the neural hemodynamic response in young, presymptomatic individuals, potentially paving the way for the development of a biomarker that could allow for earlier diagnosis.
“Our findings might be related to very early disease processes. Determining this is a task for future studies and could help to devise biomarkers for the early diagnosis of dementia. In any case, it is remarkable that a genetic predisposition for Alzheimer’s disease is already reflected in the brain at young adulthood,” explained lead author Hweeling Lee (DZNE).