Researchers turn fibroblasts into neurons for Alzheimer’s disease model
Researchers have used microRNA-based direct reprogramming to generate neurons from fibroblasts, providing new insights into late-onset Alzheimer’s disease.
Aging is the most significant risk factor for Alzheimer’s disease and as populations age, the prevalence of Alzheimer’s continues to increase globally. Understanding the influence of aging on neurons and Alzheimer’s is crucial for developing new treatments; however, studies often rely on brain biopsies. Now, researchers from the Washington University School of Medicine in St. Louis (MO, USA) have developed a method for generating aged neurons in the lab from fibroblasts of individuals with late-onset Alzheimer’s.
Sporadic, late-onset Alzheimer’s disease (LOAD) is the most common type of Alzheimer’s disease, representing more than 95% of cases. Although common, LOAD is difficult to study in the lab as it stems from various risk factors, one of the most important of which is aging. Most studies of Alzheimer’s disease have used mouse models with rare genetic mutations known to cause inherited, early-onset Alzheimer’s. However, these models do not capture the effects of aging in the development of Alzheimer’s.
To develop a model of LOAD in the lab without using brain biopsies, the team used microRNA-based direct reprogramming to generate neurons from fibroblasts from individuals with LOAD. The team cultured the LOAD neurons in a 3D environment so they self-assembled into spheroids and compared these spheroids to ones generated from people with inherited Alzheimer’s and healthy individuals of similar ages.
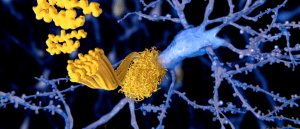 Novel microscopy technique provides insights into amyloid architecture
Novel microscopy technique provides insights into amyloid architecture
Researchers have developed a microscopy technique to visualize amyloid beta’s underlying structure, which could yield new insights into Alzheimer’s disease.
The spheroids generated from both LOAD and inherited Alzheimer’s individuals quickly developed amyloid-beta deposits and tau tangles between neurons. They found that genes associated with inflammation were activated, and the neurons began to die, which is seen in brain scans of individuals with Alzheimer’s.
The spheroids from healthy individuals showed some amyloid-beta deposits, but much less than the Alzheimer’s spheroids. This shows that the reprogrammed neurons retain the effects of aging, providing a useful model for neuronal aging. What’s more, this suggests that amyloid beta and tau accumulation correlate with aging and that Alzheimer’s disease exacerbates the process.
The researchers treated the LOAD spheroids with drugs that inhibit amyloid precursor protein processing and found that this significantly reduced amyloid deposits when treated early; however, treating after some buildup was already present had little to no effect on reducing amyloid beta deposits. This reinforces the importance of early diagnosis and treatment.
The study also found that retrotransposable elements – small pieces of DNA that jump to different locations in the genome – play a role in LOAD. To inhibit these jumping genes, the researchers treated the spheroids with the antiretroviral drug lamivudine, which can dampen the activity of retrotransposable elements. They found that the drug reduced amyloid beta deposits, tau tangles and neuronal death in the LOAD spheroids, but had no beneficial effects on the spheroids from individuals with inherited Alzheimer’s, suggesting distinct molecular features between LOAD and inherited Alzheimer’s.
“In these patients, our new model system has identified a role for retrotransposable elements associated with the disease process,” commented senior author Andrew Yoo. “We were pleased to see that we could reduce the damage with a drug treatment that suppresses these elements. We look forward to using this model system as we work towards new personalized therapeutic interventions for late-onset Alzheimer’s disease.”